Tolazoline is a potent, non-selective competitive α-adrenergic receptor antagonist. In cases of persistent pulmonary hypertension in neonates (PPHN), tolazoline, a pulmonary vasodilator, is prescribed to reduce pulmonary vascular resistance (PVR). Tolazoline exhibits both histamine agonist and mildly alpha-adrenergic blocking properties. Vascular resistance and pulmonary arterial pressure are typically lowered by tolazoline.
Physicochemical Properties
| Molecular Formula | C10H12N2 | |
| Molecular Weight | 160.21 | |
| Exact Mass | 160.1 | |
| Elemental Analysis | C, 74.97; H, 7.55; N, 17.48 | |
| CAS # | 59-98-3 | |
| Related CAS # | Tolazoline hydrochloride; 59-97-2 | |
| PubChem CID | 5504 | |
| Appearance | White to off-white solid powder | |
| Density | 1.1±0.1 g/cm3 | |
| Boiling Point | 338.2±21.0 °C at 760 mmHg | |
| Melting Point | 66-69 °C(lit.) | |
| Flash Point | 158.3±22.1 °C | |
| Vapour Pressure | 0.0±0.7 mmHg at 25°C | |
| Index of Refraction | 1.596 | |
| LogP | 2.65 | |
| Hydrogen Bond Donor Count | 1 | |
| Hydrogen Bond Acceptor Count | 1 | |
| Rotatable Bond Count | 2 | |
| Heavy Atom Count | 12 | |
| Complexity | 169 | |
| Defined Atom Stereocenter Count | 0 | |
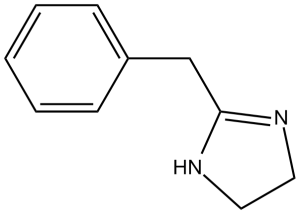
| SMILES | N1([H])C([H])([H])C([H])([H])N=C1C([H])([H])C1C([H])=C([H])C([H])=C([H])C=1[H] |
|
| InChi Key | JIVZKJJQOZQXQB-UHFFFAOYSA-N | |
| InChi Code | InChI=1S/C10H12N2/c1-2-4-9(5-3-1)8-10-11-6-7-12-10/h1-5H,6-8H2,(H,11,12) | |
| Chemical Name | 2-benzyl-4,5-dihydro-1H-imidazole | |
| Synonyms |
|
|
| HS Tariff Code | 2934.99.9001 | |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | α-adrenoceptor | |
| ln Vitro |
|
|
| ln Vivo | Studies have investigated the pharmacologic mechanism of 2-(4'-isothiocyanatobenzyl) imidazoline (IBI) and analogs for interaction with imidazoline receptors (IRs), alpha-adrenergic receptors (alpha-ARs), and calcium channels in cardiovascular muscle systems. IBI differs from tolazoline by substitution of an electrophilic isothiocyanato (NCS) group. Unlike tolazoline, which is a partial alpha-AR agonist, IBI produced an irreversible, slow-onset, and sustained contraction of rat aorta with an median effective concentration (EC50) value of 5 microM, and a maximal contraction (116%) greater than that of phenylephrine (100%) and tolazoline (59%). The IBI-induced contractions were dependent on calcium channels and independent of alpha-ARs or IRs. Similarly, structure-activity relation studies in rat aortic smooth muscles on a series of synthesized IBI analogs indicated that NCS analogs, but not those without the NCS group, exhibited effects by a non-alpha-AR, non-IR, but a calcium channel-dependent mechanism. Thus the presence of an intact IBI ring in these analogs is not a requirement for these activities. Further, IBI inhibited dihydropyridine (DHP, [3H]PN 200-110 and [3H]Bay K 8644) binding to L-type calcium channels of T-tubule membranes in rabbit skeletal muscle. In contrast to nifedipine, IBI and NCS derivatives (nifedipine-NCS, naphazoline-NCS) only partially (50-88%) displaced specific binding of these radioligands. A single site of noncooperative interaction was observed for nifedipine (nH = 0.97), whereas tolazoline-NCS (IBI, nH = 1.46) and nifedipine-NCS (nH = 1.37) exhibited a positive cooperativity in binding to DHP sites. These receptor-binding data indicate that NCS derivatives bind to L-type calcium channels and interact allosterically with DHP-binding sites. Direct binding of the NCS group to specific nucleophilic protein sites of the calcium channel may be responsible for its activation and the subsequent contractile effects of IBI. [1] | |
| Cell Assay | Tolazoline (10(-9)-10(-4) M) or sodium nitroprusside (SNP, 10(-9)-10(-4) M) were cumulatively applied on radial artery rings precontracted submaximally with noradrenaline, endothelin-1, thromboxane analogue, U46619, or potassium chloride. In addition, some rings were pretreated with tolazoline (4 x 10(-6) M) for 30 minutes and the contractile response curve to noradrenaline was assessed in its presence. Results: tolazoline effectively reversed noradrenaline-induced contractions in the radial artery, whereas it failed to produce remarkable relaxations on rings contracted with other spasmogenic agents, while SNP overcame the contractions induced by all spasmogens to a similar extent. In addition, brief pretreatment of radial artery rings with tolazoline significantly inhibited the contractions to noradrenaline. Conclusions: tolazoline is not as broadly effective as SNP against all spasmogens investigated; however, it may be effective in counteracting alpha-adrenoceptor-mediated vasospasm in human radial arteries. [2] | |
| Toxicity/Toxicokinetics |
infant TDLo intravenous 48 mg/kg/47H-C GASTROINTESTINAL: ULCERATION OR BLEEDING FROM DUODENUM; GASTROINTESTINAL: ULCERATION OR BLEEDING FROM SMALL INTESTINE Australian Paediatric Journal., 22(221), 1986 [PMID:3767790] human TDLo intravenous 150 ug/kg CARDIAC: CHANGE IN RATE; VASCULAR: OTHER CHANGES; SKIN AND APPENDAGES (SKIN): SWEATING: OTHER Folia Medica, 27(729), 1941 rat LD50 oral 1200 mg/kg Drugs in Japan, 6(511), 1982 rat LD50 intraperitoneal 100 mg/kg Drugs in Japan, 6(511), 1982 rat LD50 intravenous 85 mg/kg Drugs in Japan, 6(511), 1982 |
|
| References |
[1]. J Cardiovasc Pharmacol. 1998 May;31(5):721-33. [2]. Ann Thorac Surg. 2006 Jan;81(1):125-31. |
|
| Additional Infomation |
Tolazoline is a member of the class of imidazoles that is 4,5-dihydro-1H-imidazole substituted by a benzyl group. It has a role as an alpha-adrenergic antagonist, an antihypertensive agent and a vasodilator agent. A vasodilator that apparently has direct actions on blood vessels and also increases cardiac output. Tolazoline can interact to some degree with histamine, adrenergic, and cholinergic receptors, but the mechanisms of its therapeutic effects are not clear. It is used in treatment of persistent pulmonary hypertension of the newborn. A vasodilator that apparently has direct actions on blood vessels and also increases cardiac output. Tolazoline can interact to some degree with histamine, adrenergic, and cholinergic receptors, but the mechanisms of its therapeutic effects are not clear. It is used in treatment of persistent pulmonary hypertension of the newborn. See also: Tolazoline Hydrochloride (has salt form). Drug Indication For the treatment of pulmonary artery anomalies Mechanism of Action Vasodilation by means of a direct effect on peripheral vascular smooth muscle and indirect effects produced, in part, by release of endogenous histamine; tolazoline has moderate alpha-adrenergic blocking activity and has histamine agonist activity. Tolazoline usually reduces pulmonary arterial pressure and vascular resistance. Tolazoline hydrochloride is a member of benzenes. A vasodilator that apparently has direct actions on blood vessels and also increases cardiac output. Tolazoline can interact to some degree with histamine, adrenergic, and cholinergic receptors, but the mechanisms of its therapeutic effects are not clear. It is used in treatment of persistent pulmonary hypertension of the newborn. See also: Tolazoline (has active moiety). The radial artery is increasingly being used in coronary revascularization as an alternative conduit to a saphenous vein graft. Its perfect endothelial capacity provides a high patency rate comparable with the internal mammary artery (IMA). However, its spastic characteristics cause difficulties during its intraoperative preparation and may lead to early postoperative graft failure. Thus, treatment and/or prevention of radial artery spasm with an effective vasodilator agent is essential for its longevity. Endogenous vasoconstrictors, including noradrenaline, endothelin-1, and thromboxane A2, are likely to play a role in the pathogenesis of graft spasm. In the present study, we evaluated the vasorelaxant effect of tolazoline, a nonselective alpha-adrenoceptor blocker, against the contractions induced by various spasmogenic agents in an isolated human radial artery.[2] |
Solubility Data
| Solubility (In Vitro) |
|
|||
| Solubility (In Vivo) |
Note: Listed below are some common formulations that may be used to formulate products with low water solubility (e.g. < 1 mg/mL), you may test these formulations using a minute amount of products to avoid loss of samples. Injection Formulations (e.g. IP/IV/IM/SC) Injection Formulation 1: DMSO : Tween 80: Saline = 10 : 5 : 85 (i.e. 100 μL DMSO stock solution → 50 μL Tween 80 → 850 μL Saline) *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH ₂ O to obtain a clear solution. Injection Formulation 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL DMSO → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Injection Formulation 3: DMSO : Corn oil = 10 : 90 (i.e. 100 μL DMSO → 900 μL Corn oil) Example: Take the Injection Formulation 3 (DMSO : Corn oil = 10 : 90) as an example, if 1 mL of 2.5 mg/mL working solution is to be prepared, you can take 100 μL 25 mg/mL DMSO stock solution and add to 900 μL corn oil, mix well to obtain a clear or suspension solution (2.5 mg/mL, ready for use in animals). Injection Formulation 4: DMSO : 20% SBE-β-CD in saline = 10 : 90 [i.e. 100 μL DMSO → 900 μL (20% SBE-β-CD in saline)] *Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Injection Formulation 5: 2-Hydroxypropyl-β-cyclodextrin : Saline = 50 : 50 (i.e. 500 μL 2-Hydroxypropyl-β-cyclodextrin → 500 μL Saline) Injection Formulation 6: DMSO : PEG300 : castor oil : Saline = 5 : 10 : 20 : 65 (i.e. 50 μL DMSO → 100 μLPEG300 → 200 μL castor oil → 650 μL Saline) Injection Formulation 7: Ethanol : Cremophor : Saline = 10: 10 : 80 (i.e. 100 μL Ethanol → 100 μL Cremophor → 800 μL Saline) Injection Formulation 8: Dissolve in Cremophor/Ethanol (50 : 50), then diluted by Saline Injection Formulation 9: EtOH : Corn oil = 10 : 90 (i.e. 100 μL EtOH → 900 μL Corn oil) Injection Formulation 10: EtOH : PEG300:Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL EtOH → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Oral Formulations Oral Formulation 1: Suspend in 0.5% CMC Na (carboxymethylcellulose sodium) Oral Formulation 2: Suspend in 0.5% Carboxymethyl cellulose Example: Take the Oral Formulation 1 (Suspend in 0.5% CMC Na) as an example, if 100 mL of 2.5 mg/mL working solution is to be prepared, you can first prepare 0.5% CMC Na solution by measuring 0.5 g CMC Na and dissolve it in 100 mL ddH2O to obtain a clear solution; then add 250 mg of the product to 100 mL 0.5% CMC Na solution, to make the suspension solution (2.5 mg/mL, ready for use in animals). Oral Formulation 3: Dissolved in PEG400 Oral Formulation 4: Suspend in 0.2% Carboxymethyl cellulose Oral Formulation 5: Dissolve in 0.25% Tween 80 and 0.5% Carboxymethyl cellulose Oral Formulation 6: Mixing with food powders Note: Please be aware that the above formulations are for reference only. InvivoChem strongly recommends customers to read literature methods/protocols carefully before determining which formulation you should use for in vivo studies, as different compounds have different solubility properties and have to be formulated differently. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 6.2418 mL | 31.2090 mL | 62.4181 mL | |
| 5 mM | 1.2484 mL | 6.2418 mL | 12.4836 mL | |
| 10 mM | 0.6242 mL | 3.1209 mL | 6.2418 mL |