Reparixin (also known as Repertaxin), is a novel, potent small molecular weight allosteric inhibitor of chemokine receptor 1/2 (CXCR1/2) activation. It is the first medication candidate that is being studied in a clinical setting to prevent ischemia/reperfusion damage in organ transplant recipients. Dual allosteric CXCR1 and CXCR2 inhibitors have been designed using a computer-aided design program that took into account the mode of binding of reparixin to CXCR1. A noncompetitive allosteric mode of interaction between CXCR1 and Repertaxin, which stops signaling by locking CXCR1 in an inactive conformation, is consistent with structural and biochemical data. Repertaxin shields organs from reperfusion injury and is an efficient in vivo inhibitor of polymorphonuclear cell recruitment. One general tactic to alter chemoattractant receptor activity is to target the Repertaxin interaction site of CXCR1.
Physicochemical Properties
| Molecular Formula | C14H21NO3S | |
| Molecular Weight | 283.39 | |
| Exact Mass | 283.124 | |
| Elemental Analysis | C, 59.34; H, 7.47; N, 4.94; O, 16.94; S, 11.31 | |
| CAS # | 266359-83-5 | |
| Related CAS # | (Rac)-Reparixin; 957407-64-6; Reparixin L-lysine salt; 266359-93-7 | |
| PubChem CID | 9838712 | |
| Appearance | White to off-white solid powder | |
| Density | 1.137g/cm3 | |
| Melting Point | 103-105 ºC | |
| Index of Refraction | 1.524 | |
| LogP | 3.985 | |
| Hydrogen Bond Donor Count | 1 | |
| Hydrogen Bond Acceptor Count | 3 | |
| Rotatable Bond Count | 5 | |
| Heavy Atom Count | 19 | |
| Complexity | 389 | |
| Defined Atom Stereocenter Count | 1 | |
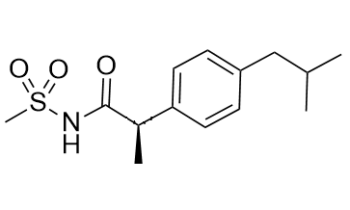
| SMILES | S(C([H])([H])[H])(N([H])C([C@]([H])(C([H])([H])[H])C1C([H])=C([H])C(=C([H])C=1[H])C([H])([H])C([H])(C([H])([H])[H])C([H])([H])[H])=O)(=O)=O |
|
| InChi Key | KQDRVXQXKZXMHP-LLVKDONJSA-N | |
| InChi Code | InChI=1S/C14H21NO3S/c1-10(2)9-12-5-7-13(8-6-12)11(3)14(16)15-19(4,17)18/h5-8,10-11H,9H2,1-4H3,(H,15,16)/t11-/m1/s1 | |
| Chemical Name | (2R)-2-[4-(2-methylpropyl)phenyl]-N-methylsulfonylpropanamide | |
| Synonyms |
|
|
| HS Tariff Code | 2934.99.9001 | |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | CXCR1wt ( IC50 = 5.6 nM ); CXCR1Ile43Val ( IC50 = 80 nM ); CXCR1 ( IC50 = 1 nM ); CXCR2 ( IC50 ∼100 nM ) | |
| ln Vitro |
|
|
| ln Vivo |
Reparixin reduces inflammatory responses in a variety of injury models by inhibiting the activation of the CXCL8 receptors, CXCR1 and CXCR2. Reparixin increases blood flow and effectively lowers systolic blood pressure. Comparing SHR-R (the reparixin-treated group) to SHR-N (the regular saline-treated SHR), the thoracic aorta wall thickness is significantly lower in the former[1]. Rats with spontaneous hypertension (SHR). Reparixin, an inhibitor of CXCL8 receptor CXCR1 and CXCR2 activation, has been shown to attenuate inflammatory responses in various injury models. In the present study, the hypertension-related functional roles of reparixin were examined in hypertensive animals. Spontaneously hypertensive rats (SHR) at the age of 18 weeks were administered a subcutaneous injection of reparixin (5 mg/kg) daily for 3 weeks (SHR-R, n=5). Control groups consisted of normal saline-treated SHR (SHR-N, n=5) and normotensive Wistar-Kyoto rats (WKY-N, n=5). Reparixin effectively decreased systolic blood pressure and increased the blood flow. The thoracic aorta wall thickness was significantly decreased in SHR-R compared to SHR-N. Expressions of CXCL8, CCL2, 12-lipoxygenase (LO) and endothelin (ET)-1 were significantly decreased in SHR-R thoracic aorta tissues compared to SHR-N. Furthermore, expression of angiotensin II subtype I receptor (AT(1)R) protein was decreased in SHR-R thoracic aorta tissues compared to SHR-N. In addition, the plasma levels of nitric oxide were slightly elevated in SHR-R compared to the levels in SHR-N. These findings indicate that inhibition of hypertension-related mediators by reparixin results in the reduction of blood pressure in SHR. Therefore, these results suggest that reparixin-mediated blockade of CXCL8 receptor activation attenuates vascular hypertension in SHR.[1] Pharmacological inhibition of CXCR2 by Reparixin reduced CXCL1-induced leukocyte arrest in the microcirculation of the cremaster muscle, but did not influence arrest in response to leukotriene B4 (LTB4) demonstrating specificity. Reparixin (15 microg g(-1)) reduced neutrophil recruitment in the lung by approximately 50% in a model of LPS-induced ALI. A higher dose did not provide additional reduction of neutrophil recruitment. This dose also reduced accumulation of neutrophils in the interstitial compartment and vascular permeability in LPS-induced ALI. Furthermore, both prophylactic and therapeutic application of Reparixin improved gas exchange, and reduced neutrophil recruitment and vascular permeability in a clinically relevant model of acid-induced ALI. Conclusions and implications: Reparixin, a non-competitive allosteric CXCR2 inhibitor attenuates ALI by reducing neutrophil recruitment and vascular permeability[2]. |
|
| Enzyme Assay | Reparixin L-lysine salt is a new and powerful small molecular weight allosteric inhibitor of chemokine receptor 1/2 (CXCR1/2) activation. It is the L-lysine salt form of reparixin. Reparixin, as demonstrated in particular experiments on CXCR1/L1.2 and CXCR2/L1.2 transfected cells and on human PMNs, is a strong functional inhibitor of CXCL8-induced biological activities on human PMNs with a marked selectivity (about 400-fold) for CXCR1. Reparixin's effectiveness is considerably reduced in L1.2 cells that express the CXCR1 Ile43Val mutant (IC50 values for CXCR1 wt and CXCR1 Ile43Val, respectively, are 5.6 nM and 80 nM). | |
| Cell Assay | L1.2 Cell suspension (1.5-3×106 cells/mL) is then seeded in triplicate in the upper compartment of the chemotactic chamber after being incubated for 15 min at 37°C with either vehicle or Reparixin (1 nM-1μM). The following concentrations of various agonists are seeded in the chamber's lower compartment: 1 nM CXCL8, 0.03 nM fMLP, 10 nM CXCL1, 2.5 nM CCL2, and 30 nM C5a. The chemotactic chamber is incubated for 45 minutes (human PMNs) or 2 hours (monocytes) at 37°C in air with 5% CO2. After the incubation period, the filter is taken out, cleaned, and stained. Five oil immersion fields are counted for each migration at a high magnification of 100×, following sample coding. Transwell filters with a pore size of 5 μm are used to assess L1.2 migration. | |
| Animal Protocol |
|
|
| References |
[1]. Biol Pharm Bull . 2011;34(1):120-7. [2]. Br J Pharmacol . 2008 Oct;155(3):357-64. [3]. Proc Natl Acad Sci U S A . 2004 Aug 10;101(32):11791-6. |
|
| Additional Infomation |
Reparixin is a monoterpenoid. Reparixin has been used in trials studying the treatment and prevention of Breast Cancer, Metastatic Breast Cancer, Pancreatectomy for Chronic Pancreatitis, Islet Transplantation in Diabetes Mellitus Type 1, and Pancreatic Islet Transplantation in Type 1 Diabetes Mellitus. Reparixin is an orally available inhibitor of CXC chemokine receptor types 1 (CXCR1) and 2 (CXCR2), with potential antineoplastic activity. Upon administration, reparixin allosterically binds to CXCR1 and prevents CXCR1 activation by its ligand interleukin 8 (IL-8 or CXCL8). This may cause cancer stem cell (CSC) apoptosis and may inhibit tumor cell progression and metastasis. CXCR1, overexpressed on CSCs, plays a key role in CSC survival and the ability of CSC to self-renew; it is also linked to tumor resistance to chemotherapy. Inhibition of the IL-8/CXCR1 interaction also potentiates the cytotoxic effect of chemotherapeutic agents. In addition, reparixin inhibits CXCR2 activation and may reduce both neutrophil recruitment and vascular permeability during inflammation or injury. Drug Indication Treatment of Coronavirus disease 2019 (COVID-19) Treatment of coronavirus disease 2019 (COVID-2019) Prevention of graft rejection The chemokine CXC ligand 8 (CXCL8)/IL-8 and related agonists recruit and activate polymorphonuclear cells by binding the CXC chemokine receptor 1 (CXCR1) and CXCR2. Here we characterize the unique mode of action of a small-molecule inhibitor (Repertaxin) of CXCR1 and CXCR2. Structural and biochemical data are consistent with a noncompetitive allosteric mode of interaction between CXCR1 and Repertaxin, which, by locking CXCR1 in an inactive conformation, prevents signaling. Repertaxin is an effective inhibitor of polymorphonuclear cell recruitment in vivo and protects organs against reperfusion injury. Targeting the Repertaxin interaction site of CXCR1 represents a general strategy to modulate the activity of chemoattractant receptors.[3] Background and purpose: Acute lung injury (ALI) remains a major challenge in critical care medicine. Both neutrophils and chemokines have been proposed as key components in the development of ALI. The main chemokine receptor on neutrophils is CXCR2, which regulates neutrophil recruitment and vascular permeability, but no small molecule CXCR2 inhibitor has been demonstrated to be effective in ALI or animal models of ALI. To investigate the functional relevance of the CXCR2 inhibitor Reparixin in vivo, we determined its effects in two models of ALI, induced by either lipopolysaccharide (LPS) inhalation or acid instillation. Experimental approach: In two ALI models in mice, we measured vascular permeability by Evans blue and evaluated neutrophil recruitment into the lung vasculature, interstitium and airspace by flow cytometry. [2] |
Solubility Data
| Solubility (In Vitro) |
|
|||
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 2.5 mg/mL (8.82 mM) (saturation unknown) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 25.0 mg/mL clear DMSO stock solution to 400 μL PEG300 and mix evenly; then add 50 μL Tween-80 to the above solution and mix evenly; then add 450 μL normal saline to adjust the volume to 1 mL. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 2: ≥ 2.5 mg/mL (8.82 mM) (saturation unknown) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 25.0 mg/mL clear DMSO stock solution to 900 μL of 20% SBE-β-CD physiological saline solution and mix evenly. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Solubility in Formulation 3: ≥ 2.5 mg/mL (8.82 mM) (saturation unknown) in 10% DMSO + 90% Corn Oil (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 25.0 mg/mL clear DMSO stock solution to 900 μL of corn oil and mix evenly. Solubility in Formulation 4: ≥ 2.5 mg/mL (8.82 mM) (saturation unknown) in 5% DMSO + 40% PEG300 + 5% Tween80 + 50% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 5: 2.5 mg/mL (8.82 mM) in 5% DMSO + 95% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), suspension solution; with ultrasonication. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.5287 mL | 17.6435 mL | 35.2871 mL | |
| 5 mM | 0.7057 mL | 3.5287 mL | 7.0574 mL | |
| 10 mM | 0.3529 mL | 1.7644 mL | 3.5287 mL |