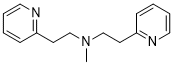
NSC19005 (Betahistine EP Impurity C) is an impurity of Betahistine and is structurally related to Betahistine. NSC19005 is a betahistine dimer. For the treatment of rheumatoid arthritis (RA), betahistine is a strong, well-tolerated, oral bioactive histamine H1 and H3 receptor agonist.
Physicochemical Properties
| Molecular Formula | C15H19N3 |
| Molecular Weight | 241.338 |
| Exact Mass | 241.158 |
| Elemental Analysis | C, 74.65; H, 7.94; N, 17.41 |
| CAS # | 5452-87-9 |
| Related CAS # | 5452-87-9 |
| PubChem CID | 227430 |
| Appearance | Solid powder |
| Density | 1.067g/cm3 |
| Boiling Point | 371.9ºC at 760mmHg |
| Flash Point | 178.7ºC |
| Index of Refraction | 1.568 |
| LogP | 2.193 |
| Hydrogen Bond Donor Count | 0 |
| Hydrogen Bond Acceptor Count | 3 |
| Rotatable Bond Count | 6 |
| Heavy Atom Count | 18 |
| Complexity | 198 |
| Defined Atom Stereocenter Count | 0 |
| SMILES | CN(CCC1=NC=CC=C1)CCC2=NC=CC=C2 |
| InChi Key | PQHKIDBZBKQYMR-UHFFFAOYSA-N |
| InChi Code | InChI=1S/C15H19N3/c1-18(12-8-14-6-2-4-10-16-14)13-9-15-7-3-5-11-17-15/h2-7,10-11H,8-9,12-13H2,1H3 |
| Chemical Name | N-methyl-2-pyridin-2-yl-N-(2-pyridin-2-ylethyl)ethanamine |
| Synonyms | NSC19005; NSC-19005; 5452-87-9; N-Methyl-2-(pyridin-2-yl)-N-(2-(pyridin-2-yl)ethyl)ethanamine; Betahistine EP Impurity C; N-Methyl-N,N-bis(2-pyridylethyl)amine; Methylbis(2-pyridylethyl)amine; NSC-19005; Betahistine impurity C; NSC 19005 |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | Betahistine impurity |
| ln Vitro | Betahistine (0-10 μM) has IC50 values of 1.9 μM and 3.3 μM, respectively, that prevent [125I]iodoproxyfan from binding to the membranes of CHO (rH3(445)R) and CHO (hH3(445)R) cells. result in Ki values that are, respectively, 2.5 μM and 1.4 μM3]. |
| References |
[1]. Characterization and in silico Mutagenic Assessment of a New Betahistine Degradation Impurity. J. Braz. Chem. Soc. vol.30 no.7 São Paulo July 2019 Epub July 04, 2019. [2]. The effect of betahistine, a histamine H1 receptor agonist/H3 antagonist, on olanzapine-induced weight gain in first-episode schizophrenia patients. Int Clin Psychopharmacol. 2005 Mar;20(2):101-3. [3]. Effects of betahistine at histamine H3 receptors: mixed inverse agonism/agonism in vitro and partial inverse agonism in vivo. J Pharmacol Exp Ther . 2010 Sep 1;334(3):945-54. |
| Additional Infomation |
Currently, the pharmaceutical industry devotes great attention to drug degradation products because these compounds can offer risks to patients. A previous degradation study of betahistine (N-α-methyl-2-pyridylethylamine) conducted under different stress conditions detected three main impurities named A, B and C. Degradation products were analyzed by high-resolution mass spectrometry in electrospray source and time of flight analyzer (ESI-TOF) and nuclear magnetic resonance (NMR). Impurity mutagenicity was evaluated by Derek Nexus and Sarah Nexus softwares. Liquid chromatography hyphenate with tandem mass spectrometry (LC-MS/MS) analysis of the betahistine forced degradation sample indicated the presence of a new impurity, which was named impurity C1. 2D NMR experiments allowed the complete structural characterization of the new entity. The active pharmaceutical ingredient and degradation impurities were classified as inactive in the in silico mutagenic studies. Systematic investigation of a forced degradation sample led to the characterization of a new betahistine impurity. The in silico mutagenicity study of the betahistine degradation impurities may be useful in the risk assessment of the drug products. [1] Histamine antagonism has been implicated in antipsychotic drug-induced weight gain. Betahistine, a histamine enhancer with H1 agonistic/H3 antagonistic properties (48 mg t.i.d.), was coadministered with olanzapine (10 mg/day) in three first-episode schizophrenia patients for 6 weeks. Body weight was measured at baseline and weekly thereafter. Clinical rating scales were completed at baseline and at week 6. All participants gained weight (mean weight gain 3.1+/-0.9 kg) and a similar pattern of weight gain was observed: an increase during the first 2 weeks and no additional weight gain (two patients) or minor weight loss (one patient) from weeks 3 to 6. None gained 7% of baseline weight, which is the cut-off for clinically significant weight gain. Betahistine was safe and well tolerated and did not interfere with the antipsychotic effect of olanzapine. Our findings justify a placebo-controlled evaluation of the putative weight-attenuating effect of betahistine in olanzapine-induced weight gain.[2] We previously suggested that therapeutic effects of betahistine in vestibular disorders result from its antagonist properties at histamine H(3) receptors (H(3)Rs). However, H(3)Rs exhibit constitutive activity, and most H(3)R antagonists act as inverse agonists. Here, we have investigated the effects of betahistine at recombinant H(3)R isoforms. On inhibition of cAMP formation and [(3)H]arachidonic acid release, betahistine behaved as a nanomolar inverse agonist and a micromolar agonist. Both effects were suppressed by pertussis toxin, were found at all isoforms tested, and were not detected in mock cells, confirming interactions at H(3)Rs. The inverse agonist potency of betahistine and its affinity on [(125)I]iodoproxyfan binding were similar in rat and human. We then investigated the effects of betahistine on histamine neuron activity by measuring tele-methylhistamine (t-MeHA) levels in the brains of mice. Its acute intraperitoneal administration increased t-MeHA levels with an ED(50) of 0.4 mg/kg, indicating inverse agonism. At higher doses, t-MeHA levels gradually returned to basal levels, a profile probably resulting from agonism. After acute oral administration, betahistine increased t-MeHA levels with an ED(50) of 2 mg/kg, a rightward shift probably caused by almost complete first-pass metabolism. In each case, the maximal effect of betahistine was lower than that of ciproxifan, indicating partial inverse agonism. After an oral 8-day treatment, the only effective dose of betahistine was 30 mg/kg, indicating that a tolerance had developed. These data strongly suggest that therapeutic effects of betahistine result from an enhancement of histamine neuron activity induced by inverse agonism at H(3) autoreceptors.[3] |
Solubility Data
| Solubility (In Vitro) | May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples |
| Solubility (In Vivo) |
Note: Listed below are some common formulations that may be used to formulate products with low water solubility (e.g. < 1 mg/mL), you may test these formulations using a minute amount of products to avoid loss of samples. Injection Formulations (e.g. IP/IV/IM/SC) Injection Formulation 1: DMSO : Tween 80: Saline = 10 : 5 : 85 (i.e. 100 μL DMSO stock solution → 50 μL Tween 80 → 850 μL Saline) *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH ₂ O to obtain a clear solution. Injection Formulation 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL DMSO → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Injection Formulation 3: DMSO : Corn oil = 10 : 90 (i.e. 100 μL DMSO → 900 μL Corn oil) Example: Take the Injection Formulation 3 (DMSO : Corn oil = 10 : 90) as an example, if 1 mL of 2.5 mg/mL working solution is to be prepared, you can take 100 μL 25 mg/mL DMSO stock solution and add to 900 μL corn oil, mix well to obtain a clear or suspension solution (2.5 mg/mL, ready for use in animals). Injection Formulation 4: DMSO : 20% SBE-β-CD in saline = 10 : 90 [i.e. 100 μL DMSO → 900 μL (20% SBE-β-CD in saline)] *Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Injection Formulation 5: 2-Hydroxypropyl-β-cyclodextrin : Saline = 50 : 50 (i.e. 500 μL 2-Hydroxypropyl-β-cyclodextrin → 500 μL Saline) Injection Formulation 6: DMSO : PEG300 : castor oil : Saline = 5 : 10 : 20 : 65 (i.e. 50 μL DMSO → 100 μLPEG300 → 200 μL castor oil → 650 μL Saline) Injection Formulation 7: Ethanol : Cremophor : Saline = 10: 10 : 80 (i.e. 100 μL Ethanol → 100 μL Cremophor → 800 μL Saline) Injection Formulation 8: Dissolve in Cremophor/Ethanol (50 : 50), then diluted by Saline Injection Formulation 9: EtOH : Corn oil = 10 : 90 (i.e. 100 μL EtOH → 900 μL Corn oil) Injection Formulation 10: EtOH : PEG300:Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL EtOH → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Oral Formulations Oral Formulation 1: Suspend in 0.5% CMC Na (carboxymethylcellulose sodium) Oral Formulation 2: Suspend in 0.5% Carboxymethyl cellulose Example: Take the Oral Formulation 1 (Suspend in 0.5% CMC Na) as an example, if 100 mL of 2.5 mg/mL working solution is to be prepared, you can first prepare 0.5% CMC Na solution by measuring 0.5 g CMC Na and dissolve it in 100 mL ddH2O to obtain a clear solution; then add 250 mg of the product to 100 mL 0.5% CMC Na solution, to make the suspension solution (2.5 mg/mL, ready for use in animals). Oral Formulation 3: Dissolved in PEG400 Oral Formulation 4: Suspend in 0.2% Carboxymethyl cellulose Oral Formulation 5: Dissolve in 0.25% Tween 80 and 0.5% Carboxymethyl cellulose Oral Formulation 6: Mixing with food powders Note: Please be aware that the above formulations are for reference only. InvivoChem strongly recommends customers to read literature methods/protocols carefully before determining which formulation you should use for in vivo studies, as different compounds have different solubility properties and have to be formulated differently. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 4.1435 mL | 20.7177 mL | 41.4353 mL | |
| 5 mM | 0.8287 mL | 4.1435 mL | 8.2871 mL | |
| 10 mM | 0.4144 mL | 2.0718 mL | 4.1435 mL |