Physicochemical Properties
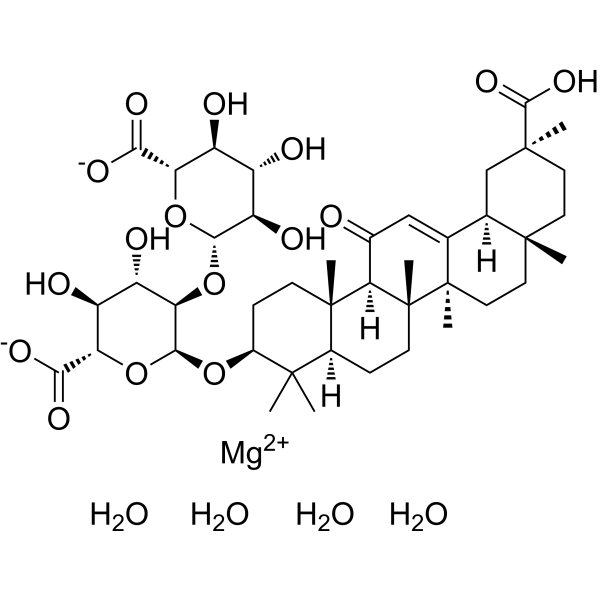
| Molecular Formula | C42H68MGO20 |
| Molecular Weight | 917.28 |
| Exact Mass | 916.415 |
| CAS # | 658701-67-8 |
| PubChem CID | 154572846 |
| Appearance | White to off-white solid powder |
| Source | liquorice plant (Glycyrrhiza glabra) |
| Hydrogen Bond Donor Count | 10 |
| Hydrogen Bond Acceptor Count | 20 |
| Rotatable Bond Count | 5 |
| Heavy Atom Count | 63 |
| Complexity | 1720 |
| Defined Atom Stereocenter Count | 19 |
| SMILES | C[C@]12CC[C@](C[C@@H]1C3=CC(=O)[C@@H]4[C@]5(CC[C@@H](C([C@@H]5CC[C@]4([C@@]3(CC2)C)C)(C)C)O[C@@H]6[C@@H]([C@H]([C@@H]([C@H](O6)C(=O)[O-])O)O)O[C@H]7[C@@H]([C@H]([C@@H]([C@H](O7)C(=O)[O-])O)O)O)C)(C)C(=O)O.O.O.O.O.[Mg+2] |
| InChi Key | NZIKWFVGLMNGAH-PUBQWMFISA-L |
| InChi Code | InChI=1S/C42H62O16.Mg.4H2O/c1-37(2)21-8-11-42(7)31(20(43)16-18-19-17-39(4,36(53)54)13-12-38(19,3)14-15-41(18,42)6)40(21,5)10-9-22(37)55-35-30(26(47)25(46)29(57-35)33(51)52)58-34-27(48)23(44)24(45)28(56-34)32(49)50;;;;;/h16,19,21-31,34-35,44-48H,8-15,17H2,1-7H3,(H,49,50)(H,51,52)(H,53,54);;4*1H2/q;+2;;;;/p-2/t19-,21+,22+,23+,24+,25+,26+,27-,28+,29+,30-,31-,34+,35+,38-,39+,40+,41-,42-;;;;;/m1...../s1 |
| Chemical Name | magnesium;(2S,3S,4S,5R,6R)-6-[(2S,3R,4S,5S,6S)-2-[[(3S,4aR,6aR,6bS,8aS,11S,12aS,14aR,14bS)-11-carboxy-4,4,6a,6b,8a,11,14b-heptamethyl-14-oxo-2,3,4a,5,6,7,8,9,10,12,12a,14a-dodecahydro-1H-picen-3-yl]oxy]-6-carboxylato-4,5-dihydroxyoxan-3-yl]oxy-3,4,5-trihydroxyoxane-2-carboxylate;tetrahydrate |
| Synonyms | Tianqingganmei; Tian qing gan mei; QX28B7638W; Magnesium isoglycyrrhizinate hydrate; Magnesium isoglycyrrhizinate (hydrate); 658701-67-8; UNII-QX28B7638W; AC-37933; |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month Note: Please store this product in a sealed and protected environment, avoid exposure to moisture. |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | Natural product from liquorice plant (Glycyrrhiza glabra); Caspase-1; NLRP3 |
| ln Vivo |
It showed that Magnesium isoglycyrrhizinate (MgIG) treatment (0.40 or 0.80 mg/kg/day) could recover the weight and the clinical symptoms of rats with COPD, accompanied with lung inflammation infiltration reduction, airway wall attenuation, bronchial mucus secretion reduction. Additionally, MgIG administration reduced inflammatory cells (white blood cells, neutrophils, lymphocytes and monocytes) accumulation in bronchoalveolar lavage fluid and decreased IL-6 and TNF-α production in the serum of COPD rats. Furthermore, MgIG treatment also reduced the expression level of NLRP3 and cleaved caspase-1.
Conclusion: It indicate that Magnesium isoglycyrrhizinate (MgIG) might be an alternative for COPD treatment, and its mechanism of action might be related to the suppression of NLRP3 inflammasome. [1]
Effect of Magnesium isoglycyrrhizinate (MgIG) on body weight, clinical symptoms and pulmonary functionin of rats with COPD. [1] The weight of rats in MDL group decreased compared with that in CON groups during 30 days of COPD rat model construction (P < 0.01, Fig. 3A). Whereas, the subsequent treatment with the low and high dose MgIG could significantly recover the growth of these rats, same as treatment with salmeterol fluticasone (P < 0.05 or P < 0.01, Fig. 3B). Compared with CON group, FEV0.3/FVC in MDL group decreased significantly (P < 0.01), which was reversed in the SMF, LOW and HIGH group significantly (Fig. 3C–E). These data suggest that 0.80 mg/kg MgIG treatment have therapeutic effects in rat with COPD.MgIG attenuates lung inflammatory responses in a rat model of COPD. Magnesium isoglycyrrhizinate (MgIG) attenuates lung inflammatory responses in a rat model of COPD [1] Inflammation plays an important role in the development of COPD. We evaluated the effect of MgIG treatment on it. Compared with CON group, the number of leukocytes, neutrophils and lymphocytes in BALF in MDL group was significantly increased. And, high and low dose of MgIG treatment significantly reversed leukocytes, neutrophils and Monocytes accumulated in BALF of the COPD rats (P < 0.05 or P < 0.01, Fig. 4A–D). The 0.80 mg/kg MgIG treatment reduced the number of lymphocytes significantly as 0.55 mg/kg salmeterol fluticasone treatment, but 0.40 mg/kg MgIG treatment did not (Fig. 4C). Magnesium isoglycyrrhizinate (MgIG) reduced proinflammatory cytokines expression in the serum of COPD rat [1] IL-6 and TNF-α are important inflammatory factors and play an important role in the progression of COPD. The levels of IL-6 and TNF-α in the serum of MDL group were significantly higher than those in CON group. In contrast, the expression of IL-6 and TNF-α were significantly suppressed by MgIG treatment (P < 0.05 or P < 0.01, Fig. 5A, B), exhibiting dose–effect relationship. It suggested that MgIG could suppress inflammation development caused by COPD. Effect of Magnesium isoglycyrrhizinate (MgIG) on histopathology in rats with COPD [1] In order to detect the pathological changes of airway structure in COPD rats, the sections of each group were stained with HE. As demonstrated in Fig. 6A, B, compared to the control group, the lungs of rats in the MDL group exhibited inflammatory cell infiltration, bronchial wall thickening and mucous plug formation, as well as expansion of the alveolar volume (Fig. 6A, B). After MgIG intervention, rats in the LOW and HIGH group exhibited some degree of improvement in pathological changes, including inflammatory cell infiltration reduction, bronchial wall thinning, mean alveoli number decrease, and alveolar dilatation and rupture alleviation (P < 0.05 or P < 0.01, Fig. 6C–E). Magnesium isoglycyrrhizinate (MgIG) suppresses the expression of NLRP3 inflammasome in COPD rats induced by cigarette and LPS [1] Western blotting analysis revealed that the expression levels of NLRP3 and cleaved caspase-1 was dramatically decreased in lung tissue of rats in LOW and HIGH groups compared to those in MDL group (P < 0.05 or P < 0.01, Fig. 7A–C). |
| Animal Protocol |
Rat model of COPD was constructed by endotracheal-atomized lipopolysaccharide exposure and cigarette smoke induction. Rats were randomly divided into 5 groups: control group, COPD model group, salmeterol fluticasone comparator group, low dose of Magnesium isoglycyrrhizinate (MgIG) group, and high dose of MgIG group. Except for normal control group, the other four groups received sensitization treatment by cigarette smoking and endotracheal-atomization of endotoxin lipopolysaccharide to construct COPD rats model. After model established successfully, the COPD rats in each group received corresponding dose of endotracheal-atomized normal saline, salmeterol fluticasone, and MgIG every day prior to exposure of cigarette smoke from days 30 to 45. Normal control group were treated with normal saline. Finally, All rats were euthanatized. Pulmonary function was measured. Cells in bronchoalveolar lavage fluid were classified, inflammatory factors IL-6 and TNF-α were determined, histopathological analysis was performed by HE staining, and expression of NLRP3 and cleaved caspase-1 in the lung tissue was also determined by Western blotting. [1]
Rat model of COPD and Magnesium isoglycyrrhizinate (MgIG) treatment.[1] The male Wistar rats (body weight, 200 ± 20 g; age, 8–10 weeks) were purchased from the Shanghai Super-B&K Laboratory Animal Co., Ltd. (Shanghai, China). The rats were housed in cages and allowed ad libitum access to rat standard diet and water throughout the experiment under the specific pathogen-free conditions with room temperature of 21–23 °C, humidity of 60 ± 5%, and a 12 h light/dark cycle. The COPD model in rats was established by cigarette smoking and endotracheal-atomization (ETA) of endotoxin lipopolysaccharide (LPS) shown in Fig. 2, according to a previous report. Rats were randomly divided into 5 groups (10 rats in each group): control group (CON), COPD model group (MDL), Salmeterol Fluticasone comparator group (SMF), low dose of Magnesium isoglycyrrhizinate (MgIG) group (LOW), High dose of MgIG group (HIGH). Rats were anesthetized with isoflurane gas on days 1 and 15 and subsequently sensitized by an endotracheal-atomization with 100 μL of 1 mg/mL LPS using liquid aerosol devices, respectively, and rats were also placed in several fumigation boxes and passively exposed to 5% (v/v) cigarette smoke produced by Hademen cigarettes, each of which contains 10 mg tar, 1.0 mg nicotine content, and 12 mg carbon monoxide, for 30 min twice with an interval of 6 h daily from days 2 to 14, except for CON group. After the COPD model rat was established successfully, rats were challenged by cigarette smoke alone with the method aforementioned every day from days 16 to 45. Additionally, SMF group received 0.55 mg/kg/d (w/bw/days) salmeterol fluticasone dissolved in normal saline, LOW group received 0.40 mg/kg/d (w/bw/days) MgIG, and High group received 0.80 mg/kg/d (w/bw/days) MgIG by endotracheal-atomization 1 h before cigarette smoke treatment from days 30 to 45, respectively, whereas MDL group received 100 μL of 0.9% normal saline with the same delivery method. Rats in CON group were sensitized and challenged with 100 μL of normal saline in the same way and exposed to the normal air. After 45 days, rats were sacrificed with an intraperitoneal injection of pentobarbital sodium (150 mg/kg). |
| References |
[1]. Magnesium isoglycyrrhizinate inhibits airway inflammation in rats with chronic obstructive pulmonary disease. BMC Pulm Med. 2021 Nov 15;21(1):371. |
| Additional Infomation |
Background:
Chronic obstructive pulmonary disease (COPD) is a kind of chronic lung diseases with the characteristics of airway remodeling and airflow obstruction. Magnesium isoglycyrrhizinate (MgIG) is an anti-inflammatory glycyrrhizic acid preparation for treating hepatitis. However, whether MgIG can treat other diseases and its action mechanism is still obscure. In this study, we evaluated the anti-inflammatory effect of MgIG in rats with COPD and investigated the underlying mechanisms.
Methods: Rat model of COPD was constructed by endotracheal-atomized lipopolysaccharide exposure and cigarette smoke induction. Rats were randomly divided into 5 groups: control group, COPD model group, salmeterol fluticasone comparator group, low dose of MgIG group, and high dose of MgIG group. Except for normal control group, the other four groups received sensitization treatment by cigarette smoking and endotracheal-atomization of endotoxin lipopolysaccharide to construct COPD rats model. After model established successfully, the COPD rats in each group received corresponding dose of endotracheal-atomized normal saline, salmeterol fluticasone, and MgIG every day prior to exposure of cigarette smoke from days 30 to 45. Normal control group were treated with normal saline. Finally, All rats were euthanatized. Pulmonary function was measured. Cells in bronchoalveolar lavage fluid were classified, inflammatory factors IL-6 and TNF-α were determined, histopathological analysis was performed by HE staining, and expression of NLRP3 and cleaved caspase-1 in the lung tissue was also determined by Western blotting. Results: It showed that MgIG treatment (0.40 or 0.80 mg/kg/day) could recover the weight and the clinical symptoms of rats with COPD, accompanied with lung inflammation infiltration reduction, airway wall attenuation, bronchial mucus secretion reduction. Additionally, MgIG administration reduced inflammatory cells (white blood cells, neutrophils, lymphocytes and monocytes) accumulation in bronchoalveolar lavage fluid and decreased IL-6 and TNF-α production in the serum of COPD rats. Furthermore, MgIG treatment also reduced the expression level of NLRP3 and cleaved caspase-1. Conclusion: It indicate that MgIG might be an alternative for COPD treatment, and its mechanism of action might be related to the suppression of NLRP3 inflammasome. [1] COPD is a common chronic lung disease which can cause some respiratory symptoms, including cough, breathlessness, and excessive phlegm. To investigate the pathophysiologic mechanism and explore potential drugs for COPD, many animal COPD models were established, among of which cigarette smoke induced rat COPD model is commonly applied. Considering difficulty in capturing both chronic bronchitis-related or emphysematous changes in a single model owing to complex COPD pathophysiology, we used LPS combined with cigarette smoke as stimuli to construct rat COPD model. The analysis result of histopathology confirmed that bronchial mucus secretion, inflammatory cells, and airway wall thickness increased in rats from MDL group. Magnesium isoglycyrrhizinate (MgIG) is a new drug for liver protection, which is obtained from glycyrrhizic acid extracted from natural plant Glycyrrhiza uralensis by alkali catalysis and isomerization. Glycyrrhiza uralensis has been used in TCM to treat lung disease for centuries due to its pharmacological and therapeutic effects. The present study investigated the suppression effect of MgIG on airway inflammatory in rats with COPD. Previous studies had indicated that long-term and/or large amounts use of glycyrrhizic acid could cause side effects, such as peseudohyperaldosteronism and hypertension, due to its hyper-mineralocorticoid-like effect. So, it is important to choose safety dosage according to mode of administration and receptor species. The intraperitoneal dose of MgIG was 100 mg/kg/day in mice, 15–45 mg/kg/day in rats, and the oral dose of MgIG was 15 mg/kg in rats, which all did not cause side effect. The mean bioavailability of glycyrrhizin in rats after intraperitoneal administration was about 80.0% [34], and the maximum observed concentration (Cmax) of MgIG in plasma was about 99.28 mg/L in health human weighed between 50.8 and 86.7 kg after intravenous administration with dosage of 300 mg dissolved in 250 mL 5% glucose. Taking these information together, we chose 0.4–0.8 mg/kg/day as endotracheal-atomization dosage in this study, and the results indicated that MgIG can alleviate the pathological changes in COPD rats, but not cause other untoward effect. Complex airway inflammation can cause airway obstruction and progressive airway remodeling in COPD rats. Various inflammatory factors and proinflammatory cytokines are involved in airway injury. Previous studies demonstrated that the serum IL-6 and TNF-α level were the key critical biomarker of COPD, which were closely correlated with the severity degree of COPD. Additionally, neutrophils enter the lungs and are activated under the action of chemokines, further aggravating the inflammatory response. Magnesium isoglycyrrhizinate (MgIG) has been indicated to have effects on anti-inflammatory and immunomodulatory activities in vitro and in vivo. In the present study, MgIG can suppress the production of proinflammatory factors TNF-α and IL-6 in the serum of COPD rats, and the increase of white blood cells, neutrophils and lymphocytes in BALF of rats in MDL group could be significantly counteracted by MgIG treatment. It means that MgIG has anti-inflammatory activity in vivo. Overall, the current results support that inhibition of airway inflammation may contribute to the protective effect of MgIG on COPD. A few studies have revealed that NLRP3 inflammasome is related to a series of chronic inflammatory diseases. Inflammasomes can recognize pathogen-associated molecular patterns (PAMPs), and then recruit and activate proinflammatory protease caspase-1, which can further cleave IL-1 β, IL-18 precursor contributing an increased secretion of proinflammatory cytokines IL-1 β and IL-18. In addition, the activation of inflammasomes can also induce cell inflammatory necrosis. In this study, the relative expression of NLRP3 and cleaved caspase-1 protein were significantly increased in the lung tissues of rats in MDL group (P < 0.05). It suggests that the mechanism of COPD may be due to the activation of NLRP3 and Cleaved caspase-1, which leads to the occurrence of COPD airway inflammation. After Magnesium isoglycyrrhizinate (MgIG) intervention treatment, the relative expression of NLRP3 and Cleaved caspase-1 proteins were significantly reduced in LOW and HIGH group as that in SMF group. That implied that MgIG can inhibit airway inflammation in COPD model rats, and its mechanism of action is associated to down-regulation of the NLRP3 signaling pathway. Limitations: COPD is a common, preventable, and treatable chronic lung disease, but its pathophysiological mechanisms is complicated. And, the clinical outcome of COPD is associated with complications it caused, such as pulmonary hypertension. Moreover, chronic consumption of glycyrrhizic acid may cause peseudohyperaldosteronism and hypertension due to its inhibition effect on 11-β-hydroxysteroid dehydrogenase type-2 (11βHSD2). So, the effect of Magnesium isoglycyrrhizinate (MgIG) on COPD needs further systematic study comprising those factors mentioned above, although we did not observe other abnormal appearance of all rats in this study. MgIG has a higher affinity to the liver after oral or injection, and it is mainly used to treat liver diseases in clinical practice. Although the method of administration in this study was pulmonary administration, avoiding the high affinity of the liver to a certain extent, individual differences in lung structure and function in rats would also affect the absorption of the drug. Additionally, state of downstream signal of the NLRP3 signaling pathway needs further evaluation to clear the effect of MgIG on NLRP3 pathway to control COPD. Conclusions: The present study demonstrated that Magnesium isoglycyrrhizinate (MgIG) attenuated pathological changes in rats with COPD by inhibiting airway inflammation and the NLRP3 signaling pathway. These findings suggest MgIG might be an alternative for COPD therapy. [1] |
Solubility Data
| Solubility (In Vitro) | H2O : 33.33 mg/mL (36.34 mM; adjust pH to 9 with NH3·H2O) |
| Solubility (In Vivo) |
Note: Listed below are some common formulations that may be used to formulate products with low water solubility (e.g. < 1 mg/mL), you may test these formulations using a minute amount of products to avoid loss of samples. Injection Formulations (e.g. IP/IV/IM/SC) Injection Formulation 1: DMSO : Tween 80: Saline = 10 : 5 : 85 (i.e. 100 μL DMSO stock solution → 50 μL Tween 80 → 850 μL Saline) *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH ₂ O to obtain a clear solution. Injection Formulation 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL DMSO → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Injection Formulation 3: DMSO : Corn oil = 10 : 90 (i.e. 100 μL DMSO → 900 μL Corn oil) Example: Take the Injection Formulation 3 (DMSO : Corn oil = 10 : 90) as an example, if 1 mL of 2.5 mg/mL working solution is to be prepared, you can take 100 μL 25 mg/mL DMSO stock solution and add to 900 μL corn oil, mix well to obtain a clear or suspension solution (2.5 mg/mL, ready for use in animals). Injection Formulation 4: DMSO : 20% SBE-β-CD in saline = 10 : 90 [i.e. 100 μL DMSO → 900 μL (20% SBE-β-CD in saline)] *Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Injection Formulation 5: 2-Hydroxypropyl-β-cyclodextrin : Saline = 50 : 50 (i.e. 500 μL 2-Hydroxypropyl-β-cyclodextrin → 500 μL Saline) Injection Formulation 6: DMSO : PEG300 : castor oil : Saline = 5 : 10 : 20 : 65 (i.e. 50 μL DMSO → 100 μLPEG300 → 200 μL castor oil → 650 μL Saline) Injection Formulation 7: Ethanol : Cremophor : Saline = 10: 10 : 80 (i.e. 100 μL Ethanol → 100 μL Cremophor → 800 μL Saline) Injection Formulation 8: Dissolve in Cremophor/Ethanol (50 : 50), then diluted by Saline Injection Formulation 9: EtOH : Corn oil = 10 : 90 (i.e. 100 μL EtOH → 900 μL Corn oil) Injection Formulation 10: EtOH : PEG300:Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL EtOH → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Oral Formulations Oral Formulation 1: Suspend in 0.5% CMC Na (carboxymethylcellulose sodium) Oral Formulation 2: Suspend in 0.5% Carboxymethyl cellulose Example: Take the Oral Formulation 1 (Suspend in 0.5% CMC Na) as an example, if 100 mL of 2.5 mg/mL working solution is to be prepared, you can first prepare 0.5% CMC Na solution by measuring 0.5 g CMC Na and dissolve it in 100 mL ddH2O to obtain a clear solution; then add 250 mg of the product to 100 mL 0.5% CMC Na solution, to make the suspension solution (2.5 mg/mL, ready for use in animals). Oral Formulation 3: Dissolved in PEG400 Oral Formulation 4: Suspend in 0.2% Carboxymethyl cellulose Oral Formulation 5: Dissolve in 0.25% Tween 80 and 0.5% Carboxymethyl cellulose Oral Formulation 6: Mixing with food powders Note: Please be aware that the above formulations are for reference only. InvivoChem strongly recommends customers to read literature methods/protocols carefully before determining which formulation you should use for in vivo studies, as different compounds have different solubility properties and have to be formulated differently. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.0902 mL | 5.4509 mL | 10.9018 mL | |
| 5 mM | 0.2180 mL | 1.0902 mL | 2.1804 mL | |
| 10 mM | 0.1090 mL | 0.5451 mL | 1.0902 mL |