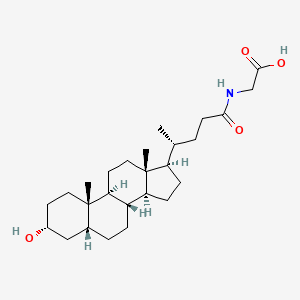
Glycolithocholic acid (Lithocholic acid glycine conjugate; Lithocholylglycine) is a glycine conjugate (N-acylglycine) of lithocholic acid which is a secondary bile acid. It is a bile acid glycine conjugate derived from a lithocholic acid.
Physicochemical Properties
| Molecular Formula | C26H43NO4 |
| Molecular Weight | 433.63 |
| Exact Mass | 433.319 |
| Elemental Analysis | C, 72.02; H, 10.00; N, 3.23; O, 14.76 |
| CAS # | 474-74-8 |
| Related CAS # | 24404-83-9 (mono-hydrochloride salt) |
| PubChem CID | 115245 |
| Appearance | White to off-white solid powder |
| Density | 1.112g/cm3 |
| Boiling Point | 619.7ºC at 760mmHg |
| Melting Point | 212-214°C (lit.) |
| Flash Point | 328.6ºC |
| LogP | 5.014 |
| Hydrogen Bond Donor Count | 3 |
| Hydrogen Bond Acceptor Count | 4 |
| Rotatable Bond Count | 6 |
| Heavy Atom Count | 31 |
| Complexity | 695 |
| Defined Atom Stereocenter Count | 9 |
| SMILES | C[C@H](CCC(=O)NCC(=O)O)[C@H]1CC[C@@H]2[C@@]1(CC[C@H]3[C@H]2CC[C@H]4[C@@]3(CC[C@H](C4)O)C)C |
| InChi Key | XBSQTYHEGZTYJE-OETIFKLTSA-N |
| InChi Code | InChI=1S/C26H43NO4/c1-16(4-9-23(29)27-15-24(30)31)20-7-8-21-19-6-5-17-14-18(28)10-12-25(17,2)22(19)11-13-26(20,21)3/h16-22,28H,4-15H2,1-3H3,(H,27,29)(H,30,31)/t16-,17-,18-,19+,20-,21+,22+,25+,26-/m1/s1 |
| Chemical Name | 2-[[(4R)-4-[(3R,5R,8R,9S,10S,13R,14S,17R)-3-hydroxy-10,13-dimethyl-2,3,4,5,6,7,8,9,11,12,14,15,16,17-tetradecahydro-1H-cyclopenta[a]phenanthren-17-yl]pentanoyl]amino]acetic acid |
| Synonyms | Lithocholic acid glycine conjugate; Lithocholylglycine; Glycolithocholic acid; Lithocholylglycine; 474-74-8; Lithocholic acid glycine conjugate; Glycine, N-[(3a,5b)-3-hydroxy-24-oxocholan-24-yl]-; Q53GV75CJG; CHEMBL258818; CHEBI:37998; Glycolithocholic acid |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | Endogenous metabolite; glycine-conjugated secondary bile acid |
| ln Vitro | Lithocholic acid (LCA) is a bile acid associated with adverse effects, including cholestasis, and it exists in vivo mainly as conjugates known as Glycolithocholic acid/glyco-LCA (GLCA) and tauro-LCA (TLCA). Tamoxifen has been linked to the development of cholestasis, and it inhibits sulfotransferase 2A1 (SULT2A1)-catalyzed dehydroepiandrosterone (DHEA) sulfonation. The present study was done to characterize the sulfonation of LCA, GLCA, and TLCA and to investigate whether triphenylethylene (clomifene, tamoxifen, toremifene, ospemifene, droloxifene), benzothiophene (raloxifene, arzoxifene), tetrahydronaphthalene (lasofoxifene, nafoxidine), indole (bazedoxifene), and benzopyran (acolbifene) classes of selective estrogen receptor modulator (SERM) inhibit LCA, GLCA, and TLCA sulfonation. Human recombinant SULT2A1, but not SULT2B1b or SULT1E1, catalyzed LCA, GLCA, and TLCA sulfonation, whereas each of these enzymes catalyzed DHEA sulfonation. LCA, GLCA, and TLCA sulfonation is catalyzed by human liver cytosol, and SULT2A1 followed the substrate inhibition model with comparable apparent K m values (≤1 µM). Each of the SERMs inhibited LCA, GLCA, and TLCA sulfonation with varying potency and mode of enzyme inhibition. The potency and extent of inhibition of LCA sulfonation were attenuated or increased by structural modifications to toremifene, bazedoxifene, and lasofoxifene. The inhibitory effect of raloxifene, bazedoxifene, and acolbifene on LCA sulfonation was also observed in HepG2 human hepatocellular carcinoma cells. Overall, among the SERMs investigated, bazedoxifene and raloxifene were the most effective inhibitors of LCA, GLCA, and TLCA sulfonation. These findings provide insight into the structural features of specific SERMs that contribute to their inhibition of SULT2A1-catalyzed LCA sulfonation. Inhibition of LCA, GLCA, and TLCA detoxification by a SERM may provide a biochemical basis for adverse effects associated with a SERM [3]. |
| ln Vivo |
In the patients with heterozygous FH type IIa, we observed both a significant decrease in the molar percentages of glycochenodeoxycholic acid, glycoursodeoxycholic acid, and Glycolithocholic acid, and a significant increase of taurochenodeoxycholic acid compared to the corresponding values in the controls. Bile analysis of six patients was reexamined during probucol treatment after 16 weeks. Probucol significantly lowered serum cholesterol levels. However, biliary lipid composition and individual bile acid proportions was not altered by the treatment. The results suggest that most of the patients with heterozygous FH have supersaturated bile and are predisposed to cholesterol gallstone formation. In addition, the mechanism by which probucol lowers serum cholesterol appears to be independent of any change in the metabolism of biliary lipid.[1] Results: Thirty-two UC patients and twenty-three HCs were enrolled in this study. It was found that the diversity of gut microbiota in UC patients was reduced compared with that in HCs. Firmicutes, Clostridium IV, Butyricicoccus, Clostridium XlVa, Faecalibacterium, and Roseburia were significantly decreased in patients with UC (P = 3.75E-05, P = 8.28E-07, P = 0.0002, P = 0.003, P = 0.0003, and P = 0.0004, respectively). Proteobacteria, Escherichia, Enterococcus, Klebsiella, and Streptococcus were significantly enriched in the UC group (P = 2.99E-09, P = 3.63E-05, P = 8.59E-05, P = 0.003, and P = 0.016, respectively). The concentrations of fecal secondary BAs, such as lithocholic acid, deoxycholic acid, glycodeoxycholic acid, Glycolithocholic acid, and taurolithocholate, in UC patients were significantly lower than those in HCs (P = 8.1E-08, P = 1.2E-07, P = 3.5E-04, P = 1.9E-03, and P = 1.8E-02, respectively) and were positively correlated with Butyricicoccus, Roseburia, Clostridium IV, Faecalibacterium, and Clostridium XlVb (P < 0.01). The concentrations of primary BAs, such as taurocholic acid, cholic acid, taurochenodeoxycholate, and glycochenodeoxycholate, in UC patients were significantly higher than those in HCs (P = 5.3E-03, P = 4E-02, P = 0.042, and P = 0.045, respectively) and were positively related to Enterococcus, Klebsiella, Streptococcus, Lactobacillus, and pro-inflammatory cytokines (P < 0.01). The expression of TGR5 was significantly elevated in UC patients (0.019 ± 0.013 vs 0.006 ± 0.003, P = 0.0003). VDR expression in colonic mucosal specimens was significantly decreased in UC patients (0.011 ± 0.007 vs 0.016 ± 0.004, P = 0.033). Conclusion: Fecal BA profiles are closely related to the gut microbiota and serum inflammatory cytokines. Dysregulation of the gut microbiota and altered constitution of fecal BAs may participate in regulating inflammatory responses via the BA receptors TGR5 and VDR [2]. |
| Enzyme Assay |
Optimization of the LCA, GLCA/Glycolithocholic acid, TLCA, and DHEA Sulfonation Assays [3] LCA sulfonation assay in human liver cytosol was optimized previously (Bansal and Lau, 2016a). LCA and GLCA/Glycolithocholic acid sulfonation increased linearly up to 100 µg of cytosolic protein, whereas TLCA sulfonation increased linearly up to 80 µg of cytosolic protein (Supplemental Fig. S1, A–C). LCA, GLCA, and TLCA sulfonation catalyzed by recombinant SULT2A1 was linear up to 5 µg of enzyme (Supplemental Fig. S1, D–F). LCA sulfonation catalyzed by human liver cytosol was linear up to 45 minutes, whereas GLCA.. |
| Animal Protocol | Background: Gut microbiota and its metabolites may be involved in the pathogenesis of inflammatory bowel disease. Several clinical studies have recently shown that patients with ulcerative colitis (UC) have altered profiles of fecal bile acids (BAs). It was observed that BA receptors Takeda G-protein-coupled receptor 5 (TGR5) and vitamin D receptor (VDR) participate in intestinal inflammatory responses by regulating NF-ĸB signaling. We hypothesized that altered profiles of fecal BAs might be correlated with gut microbiota and inflammatory responses in patients with UC. Aim: To investigate the changes in fecal BAs and analyze the relationship of BAs with gut microbiota and inflammation in patients with UC. Methods: The present study used 16S rDNA sequencing technology to detect the differences in the intestinal flora between UC patients and healthy controls (HCs). Fecal BAs were measured by targeted metabolomics approaches. Mucosal TGR5 and VDR expression was analyzed using immunohistochemistry, and serum inflammatory cytokine levels were detected by ELISA.[2] |
| References |
[1]. Biliary lipid composition in heterozygous familial hypercholesterolemia and influence of treatment with probucol. Dig Dis Sci. 1994 Jul;39(7):1586-91. [2]. Altered profiles of fecal bile acids correlate with gut microbiota and inflammatory responses in patients with ulcerative colitis. World J Gastroenterol. 2021 Jun 28;27(24):3609-3629. [3]. Inhibition of Human Sulfotransferase 2A1-Catalyzed Sulfonation of Lithocholic Acid, Glycolithocholic Acid, and Taurolithocholic Acid by Selective Estrogen Receptor Modulators and Various Analogs and Metabolites. J Pharmacol Exp Ther. 2019 Jun;369(3):389-405. [4]. Potent suppression of hydrophobic bile acids by aldafermin, an FGF19 analogue, across metabolic and cholestatic liver diseases. JHEP Rep. 2021 Feb 19;3(3):100255. |
| Additional Infomation |
Glycolithocholic acid is the glycine conjugate of lithocholic acid. It is a bile acid glycine conjugate and a N-acylglycine. It is functionally related to a lithocholic acid. It is a conjugate acid of a glycolithocholate. Glycolithocholic acid has been reported in Homo sapiens and Bos taurus with data available. See also: Glycolithocholate (annotation moved to). Background & aims: Higher serum bile acid levels are associated with an increased risk of cirrhosis and liver-related morbidity and mortality. Herein, we report secondary analyses of aldafermin, an engineered analogue of the gut hormone fibroblast growth factor 19, on the circulating bile acid profile in prospective, phase II studies in patients with metabolic or cholestatic liver disease. Methods: One hundred and seventy-six patients with biopsy-confirmed non-alcoholic steatohepatitis (NASH) and fibrosis and elevated liver fat content (≥8% by magnetic resonance imaging-proton density fat fraction) received 0.3 mg (n = 23), 1 mg (n = 49), 3 mg (n = 49), 6 mg (n = 28) aldafermin or placebo (n = 27) for 12 weeks. Sixty-two patients with primary sclerosing cholangitis (PSC) and elevated alkaline phosphatase (>1.5× upper limit of normal) received 1 mg (n = 21), 3 mg (n = 21) aldafermin or placebo (n = 20) for 12 weeks. Serum samples were collected on day 1 and week 12 for determination of bile acid profile and neoepitope-specific N-terminal pro-peptide of type III collagen (Pro-C3), a direct measure of fibrogenesis. Results: Treatment with aldafermin resulted in significant dose-dependent reductions in serum bile acids. In particular, bile acids with higher hydrophobicity indices, such as deoxycholic acid, lithocholic acid, glycodeoxycholic acid, glycochenodeoxycholic acid, and glycocholic acid, were markedly lowered by aldafermin in both NASH and PSC populations. Moreover, aldafermin predominantly suppressed the glycine-conjugated bile acids, rather than the taurine-conjugated bile acids. Changes in levels of bile acids correlated with changes in the novel fibrogenesis marker Pro-C3, which detects a neo-epitope of the type III collagen during its formation, in the pooled NASH and PSC populations. Conclusions: Aldafermin markedly reduced major hydrophobic bile acids that have greater detergent activity and cytotoxicity. Our data provide evidence that bile acids may contribute to sustaining a pro-fibrogenic microenvironment in the liver across metabolic and cholestatic liver diseases. Lay summary: Aldafermin is an analogue of a gut hormone, which is in development as a treatment for patients with chronic liver disease. Herein, we show that aldafermin can potently and robustly suppress the toxic, hydrophobic bile acids irrespective of disease aetiology. The therapeutic strategy utilising aldafermin may be broadly applicable to other chronic gastrointestinal and liver disorders. Clinical trials registration: The study is registered at Clinicaltrials.govNCT02443116 and NCT02704364.[4] |
Solubility Data
| Solubility (In Vitro) | DMSO : ~50 mg/mL (~115.31 mM) |
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 1.25 mg/mL (2.88 mM) (saturation unknown) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 12.5 mg/mL clear DMSO stock solution to 900 μL of 20% SBE-β-CD physiological saline solution and mix evenly. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Solubility in Formulation 2: ≥ 1.25 mg/mL (2.88 mM) (saturation unknown) in 10% DMSO + 90% Corn Oil (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 12.5 mg/mL clear DMSO stock solution to 900 μL of corn oil and mix evenly. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.3061 mL | 11.5306 mL | 23.0611 mL | |
| 5 mM | 0.4612 mL | 2.3061 mL | 4.6122 mL | |
| 10 mM | 0.2306 mL | 1.1531 mL | 2.3061 mL |