Physicochemical Properties
| Molecular Formula | C19H27NAO5S |
| Molecular Weight | 390.47 |
| Exact Mass | 390.147 |
| CAS # | 1099-87-2 |
| PubChem CID | 12594 |
| Appearance | Solid powder |
| Melting Point | 148-149 °C (dec.)(lit.) |
| Index of Refraction | 10 ° (C=4, MeOH) |
| LogP | 4.444 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 5 |
| Rotatable Bond Count | 2 |
| Heavy Atom Count | 25 |
| Complexity | 721 |
| Defined Atom Stereocenter Count | 6 |
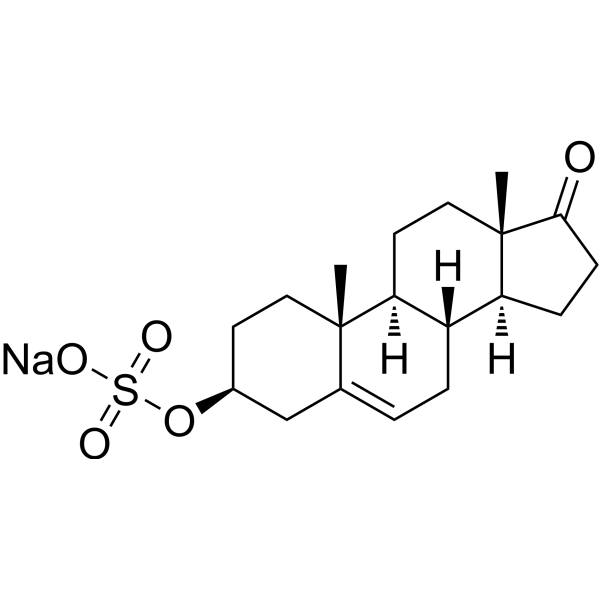
| SMILES | C[C@@]12CC[C@@H](CC2=CC[C@H]3[C@@H]4CCC(=O)[C@@]4(C)CC[C@@H]31)OS(=O)(=O)[O-].[Na+] |
| InChi Key | CZWCKYRVOZZJNM-USOAJAOKSA-N |
| InChi Code | InChI=1S/C19H28O5S/c1-18-9-7-13(24-25(21,22)23)11-12(18)3-4-14-15-5-6-17(20)19(15,2)10-8-16(14)18/h3,13-16H,4-11H2,1-2H3,(H,21,22,23)/t13-,14-,15-,16-,18-,19-/m0/s1 |
| Chemical Name | [(3S,8R,9S,10R,13S,14S)-10,13-dimethyl-17-oxo-1,2,3,4,7,8,9,11,12,14,15,16-dodecahydrocyclopenta[a]phenanthren-3-yl] hydrogen sulfate |
| Synonyms | Sodium prasterone sulfate; sodium prasterone sulfate; Prasterone sodium sulfate; 1099-87-2; Teloin; Sodium dehydroepiandrosterone sulfate; Mylis; Dehydroepiandrosterone sulfate sodium salt; Dehydroepiandrosterone sulfate sodium; |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month Note: Please store this product in a sealed and protected environment, avoid exposure to moisture. |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | Human Endogenous Metabolite |
| ln Vitro | Dehydroepiandrosterone sulfate (DHEAS) is the most abundant circulating steroid in human, with the highest concentrations between age 20 and 30, but displaying a significant decrease with age. Many beneficial functions are ascribed to DHEAS. Nevertheless, long-term studies are very scarce concerning the intake of DHEAS over several years, and molecular investigations on DHEAS action are missing so far. In this study, the role of DHEAS on the first and rate-limiting step of steroid hormone biosynthesis was analyzed in a reconstituted in vitro system, consisting of purified CYP11A1, adrenodoxin and adrenodoxin reductase. DHEAS enhances the conversion of cholesterol by 26%. Detailed analyses of the mechanism of DHEAS action revealed increased binding affinity of cholesterol to CYP11A1 and enforced interaction with the electron transfer partner, adrenodoxin. Difference spectroscopy showed K(d)-values of 40 ± 2.7 µM and 24.8 ± 0.5 µM for CYP11A1 and cholesterol without and with addition of DHEAS, respectively. To determine the K(d)-value for CYP11A1 and adrenodoxin, surface plasmon resonance measurements were performed, demonstrating a K(d)-value of 3.0 ± 0.35 nM (with cholesterol) and of 2.4 ± 0.05 nM when cholesterol and DHEAS were added. Kinetic experiments showed a lower Km and a higher kcat value for CYP11A1 in the presence of DHEAS leading to an increase of the catalytic efficiency by 75%. These findings indicate that DHEAS affects steroid hormone biosynthesis on a molecular level resulting in an increased formation of pregnenolone. [1] |
| Enzyme Assay | Sodium dehydroepiandrosterone sulfate is an organic sodium salt that is the monosodium salt of dehydroepiandrosterone sulfate. It has a role as a human metabolite and an EC 2.7.1.33 (pantothenate kinase) inhibitor. It contains a dehydroepiandrosterone sulfate(1-). |
| ADME/Pharmacokinetics |
Metabolism / Metabolites Dehydroepiandrosterone sulfate (DHEAS) is the sulfate ester of DHEA. This conversion is reversibly catalyzed by sulfotransferase (SULT2A1) primarily in the adrenals, the liver, and small intestine. DHEA sulfate can also be back-converted to DHEA through the action of steroid sulfatase. In the blood, most DHEA is found as DHEAS with levels that are about 300 times higher than those of free DHEA. Orally ingested DHEA is converted to its sulfate when passing through intestines and liver. DHEAS levels show no diurnal variation. In males and females, conversion of DHEAS to DHEA and then to testosterone requires the enzyme 17β-hydroxysteroid dehydrogenase. |
| Toxicity/Toxicokinetics |
Toxicity Summary Although it predominantly functions as an endogenous precursor to more potent androgens such as testosterone and dihydroxytestosterone, DHEA (which is produced from DHEAS) has been found to possess some degree of androgenic activity in its own right, acting as a low affinity (Ki = 1 μM), weak partial agonist of the androgen receptor. DHEA has also been found to bind to and activate the ERα and ERβ estrogen receptors with Ki values of 1.1 μM and 0.5 μM, respectively. When taken in sufficient quantities DHEAS can cause masculinizing effects. DHEAS is considered an androgenic steroid precursor because testosterone (its product) is an androgen or male hormone. In males and females, conversion of DHEAS to testosterone requires the enzyme 17β-hydroxysteroid dehydrogenase. Testosterone plays a key role in the development of male reproductive tissues such as the testis and prostate as well as promoting secondary sexual characteristics such as increased muscle, bone mass, and the growth of body hair. High levels of testosterone can lead to masculinization in females or premature puberty in young boys. Chronically high levels in adults increase the incidence of heart attack, stroke and blood clots by lowering the level of HDL (good cholesterol). The development of breast tissue in males, a condition called gynecomastia (which is usually caused by high levels of circulating estradiol), arises because of increased conversion of testosterone to estradiol by the enzyme aromatase. Reduced sexual function and temporary infertility can also occur in males. women TDLo intravenous 4 mg/kg GASTROINTESTINAL: NAUSEA OR VOMITING; SKIN AND APPENDAGES (SKIN): DERMATITIS, OTHER: AFTER SYSTEMIC EXPOSURE Japan Medical Gazette., 18(5)(10), 1981 rat LD50 oral >10 gm/kg Drugs in Japan, 6(687), 1982 rat LD50 intraperitoneal 523 mg/kg BEHAVIORAL: ALTERED SLEEP TIME (INCLUDING CHANGE IN RIGHTING REFLEX); BEHAVIORAL: ATAXIA Kiso to Rinsho. Clinical Report., 10(1852), 1976 rat LD50 intravenous 468 mg/kg BEHAVIORAL: CONVULSIONS OR EFFECT ON SEIZURE THRESHOLD; BEHAVIORAL: ATAXIA; LUNGS, THORAX, OR RESPIRATION: DYSPNEA Kiso to Rinsho. Clinical Report., 10(1852), 1976 rat LD50 intravaginal >500 mg/kg Oyo Yakuri. Pharmacometrics., 48(189), 1994 |
| References |
[1]. Dehydroepiandrosterone Sulfate (DHEAS) Stimulates the First Step in the Biosynthesis of Steroid Hormones. PLoS One. 2014 Feb 21;9(2):e89727. |
| Additional Infomation |
Dehydroepiandrosterone sulfate is a steroid sulfate that is the 3-sulfooxy derivative of dehydroepiandrosterone. It has a role as an EC 2.7.1.33 (pantothenate kinase) inhibitor, a human metabolite and a mouse metabolite. It is a steroid sulfate and a 17-oxo steroid. It is functionally related to a dehydroepiandrosterone. It is a conjugate acid of a dehydroepiandrosterone sulfate(1-). DHEA sulfate is the major steroid of the fetal adrenal. DHEA-S is the principal adrenal androgen and is secreted together with cortisol under the control of ACTH and prolactin. DHEA-S is elevated with hyperprolactinemia. Dehydroepiandrosterone sulfate has been reported in Homo sapiens and Apis cerana with data available. Dehydroepiandrosterone sulfate or DHEAS is the sulfated form of dehydroepiandrosterone (DHEA). This sulfation is reversibly catalyzed by sulfotransferase 2A1 (SULT2A1) primarily in the adrenals, the liver, and small intestine. In the blood, most DHEA is found as DHEAS with levels that are about 300 times higher than those of free DHEA. Orally-ingested DHEA is converted to its sulfate when passing through intestines and liver. Whereas DHEA levels naturally reach their peak in the early morning hours, DHEAS levels show no diurnal variation. From a practical point of view, measurement of DHEAS is preferable to DHEA, as levels are more stable. DHEA (from which DHEAS comes from) is a natural steroid prohormone produced from cholesterol by the adrenal glands, the gonads, adipose tissue, brain and in the skin (by an autocrine mechanism). DHEA is the precursor of androstenedione, which can undergo further conversion to produce the androgen testosterone and the estrogens estrone and estradiol. DHEA is also a potent sigma-1 agonist. DHEAS can serve as a precursor for testosterone; androstenedione; estradiol; and estrone. Serum dehydroepiandrosterone sulfate is a classic marker for adrenarche and, subsequently, for the individual hormonal milieu Dehydroepiandrosterone sulfate is an endogenously produced sex steroid that has been hypothesized to have anti aging effects It also has been inversely associated with development of atherosclerosis (A3325, A3326, A3327). DHEA-S is the principal adrenal androgen and is secreted together with cortisol under the control of ACTH and prolactin. DHEA-S is elevated with hyperprolactinemia. The circulating form of a major C19 steroid produced primarily by the ADRENAL CORTEX. DHEA sulfate serves as a precursor for TESTOSTERONE; ANDROSTENEDIONE; ESTRADIOL; and ESTRONE. Drug Indication Investigated for use/treatment in asthma and burns and burn infections. Mechanism of Action The low levels of dehydroepiandrosterone sulfate(DHEA-S)is associated with unfavorable levels of several strong cardiovascular disease risk factors, such as lipids and blood pleasure, which are components of the metabolic syndrome, and insulin levels. DHEA-S deficiency is risk factors of obesity and insulin resistance, but it is not clear, whether this possible influence is independent. |
Solubility Data
| Solubility (In Vitro) |
DMSO : 100 mg/mL (256.10 mM; with sonication) H2O : 10 mg/mL (25.61 mM; with sonication) |
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 2.08 mg/mL (5.33 mM)(Saturation unknown) in 10% DMSO 40% PEG300 5% Tween-80 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution, add 100 μL of 20.8 mg/mL clear DMSO stock solution to 400 μL PEG300 and mix well; then add 50 μL Tween-80 to the above system and mix well; then add 450 μL saline to make up to 1 mL. *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 2: ≥ 2.08 mg/mL (5.33 mM)(Saturation unknown) in 10% DMSO 90% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution, add 100 μL of 20.8 mg/mL clear DMSO stock solution to 900 μL of 20% SBE-β-CD in saline and mix well. *Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Solubility in Formulation 3: ≥ 2.08 mg/mL (5.33 mM)(Saturation unknown) in 10% DMSO 90% Corn Oil (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution, add 100 μL of 20.8 mg/mL clear DMSO stock solution to 900 μL corn oil and mix well. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5610 mL | 12.8051 mL | 25.6102 mL | |
| 5 mM | 0.5122 mL | 2.5610 mL | 5.1220 mL | |
| 10 mM | 0.2561 mL | 1.2805 mL | 2.5610 mL |