Physicochemical Properties
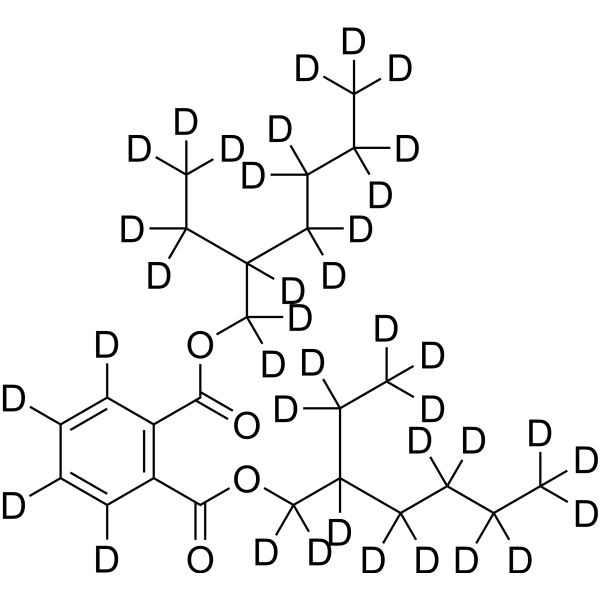
| Molecular Formula | C24D38O4 |
| Molecular Weight | 428.79 |
| Exact Mass | 428.515 |
| CAS # | 352431-42-6 |
| Related CAS # | DEHP;117-81-7 |
| PubChem CID | 8343 |
| Appearance | Colorless to light yellow liquid |
| Density | 1.0±0.1 g/cm3 |
| Boiling Point | 384.9±10.0 °C at 760 mmHg |
| Melting Point |
-58 °F (NTP, 1992) -55 °C -50 °C -58 °F -58 °F |
| Flash Point | 207.2±0.0 °C |
| Vapour Pressure | 0.0±0.9 mmHg at 25°C |
| Index of Refraction | 1.489 |
| LogP | 8.71 |
| Hydrogen Bond Donor Count | 0 |
| Hydrogen Bond Acceptor Count | 4 |
| Rotatable Bond Count | 16 |
| Heavy Atom Count | 28 |
| Complexity | 394 |
| Defined Atom Stereocenter Count | 0 |
| SMILES | C1(=C([2H])C(C(OC([2H])([2H])C([2H])(C([2H])([2H])C([2H])([2H])[2H])C([2H])([2H])C([2H])([2H])C([2H])([2H])C([2H])([2H])[2H])=O)=C(C(OC([2H])([2H])C([2H])(C([2H])([2H])C([2H])([2H])[2H])C([2H])([2H])C([2H])([2H])C([2H])([2H])C([2H])([2H])[2H])=O)C([2H])=C1[2H])[2H] |
| InChi Key | BJQHLKABXJIVAM-UHFFFAOYSA-N |
| InChi Code | InChI=1S/C24H38O4/c1-5-9-13-19(7-3)17-27-23(25)21-15-11-12-16-22(21)24(26)28-18-20(8-4)14-10-6-2/h11-12,15-16,19-20H,5-10,13-14,17-18H2,1-4H3 |
| Chemical Name | bis(2-ethylhexyl) benzene-1,2-dicarboxylate |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| ln Vitro | Drug compounds have included stable heavy isotopes of carbon, hydrogen, and other elements, mostly as quantitative tracers while the drugs were being developed. Because deuteration may have an effect on a drug's pharmacokinetics and metabolic properties, it is a cause for concern [1]. |
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion When administered either IV or orally ... it is mainly excreted in urine and bile. It appeared to be rapidly cleared from blood, most being removed within 5-7 hr of completion of dialysis. In one study of subjects who received hemodialysis, blood transfusions or blood that had previously been in contact with polyvinyl chloride medical products, di(2-ethylhexyl) phthalate was found at the following levels (ug/g wet tissue): brain (1.9), heart (0.5), kidney (1.2-2.2), liver (1.5-4.6), lung (1.4-2.2) & spleen (2.2-4.7). The levels of di(2-ethylhexyl) phthalate in neonatal heart tissue from infants who had undergone umbilical catheterization, either alone or with admin of blood products, were reported to be higher than those in similar tissue from untreated infants. For more Absorption, Distribution and Excretion (Complete) data for BIS(2-ETHYLHEXYL) PHTHALATE (67 total), please visit the HSDB record page. Metabolism / Metabolites It is hypothesized that the teratogen di(2-ethylhexyl) phthalate (DEHP) acts by in vivo hydrolysis to 2-ethylhexanol (2-EXHO), which in turn is metabolized to 2-ethylhexanoic acid (2-EXHA), the proximate teratogen. Teratological studies were conducted with Wistar rats, with administration of these agents on day 12 of geatation. On an equimolar basis DEHP was least potent, 2-ethylhexanol was intermediate, and 2-ethylhexanoic acid was the most potent of the three agents, which is consistent with the hypothesis. Similarity in the types of defects found with these agents also suggests a common mechanism, with 2-ethylhexanoic acid as the proximate teratogen. When admin either iv or orally, it is rapidly metabolized to derivatives of mono-(2-ethylhexyl)-phthalate. ... Rats have been reported to metabolize di(2-ethylhexyl) phthalate to 5-keto-2-ethylhexyl phthalate, 5-carboxyl-2-ethylpentyl phthalate, 5-hydroxy-2-ethylhexyl phthalate & 2-carboxymethylbutyl phthalate after initial hydrolysis to mono(2-ethylhexyl) phthalate. African green monkeys & ferrets, in contrast to rats, excrete di(2-ethylhexyl) phthalate metabolites in urine as glucuronide derivatives of mono(2-ethylhexyl) phthalate. Glucuronidation appears to occur at the free carboxyl group, while 2-ethylhexyl substituent is oxidized to an alcohol. For more Metabolism/Metabolites (Complete) data for BIS(2-ETHYLHEXYL) PHTHALATE (41 total), please visit the HSDB record page. DEHP is mainly absorbed via ingestion. It is hydrolyzed in the small intestine and absorbed as monoethylhexylphthalate (MEHP) and 2-ethylhexanol, then likely distributed to the adipose tissues and kidneys. MEHP is further metabolized via numerous oxidative reactions, resulting in the formation of 30 or more metabolites, some of which can be conjugated with glucuronic acid for excretion. Oxidation of 2-ethylhexanol primarily yields 2-ethylhexanoic acid and several keto acid derivatives. Most DEHP metabolites are excreted in the urine as glucuronide conjugates, while unmetabolized DEHP is excreted in the faeces. (L181) Biological Half-Life The levels of DEHP and MEHP in plasma have been studied in newborn infants given blood exchange transfusions. In one case the MEHP half-life was the same as for DEHP (about 12 hr), indicating that the hydrolysis of DEHP was the rate-limiting metabolic step. However, in other children the half-time of MEHP was longer than that of DEHP ... . After the iv admin of radiolabelled DEHP, at least two elimination phases of radioactivity, with short half-lives (4.5-9 and 22 min, respectively), were observed in rat blood ... After 7 wk of oral admin, the elimination phase in the liver was considerably slower, the half-life being 3-5 days ... No accumulation of DEHP or MEHP was observed when the dosage was 2.8 g/kg/day for 7 days ... nor was there any in a long-term (5-7 weeks) feeding study at a dose level of 1 or 5 g/kg diet (corresponding to a daily dose of about 50 and 250 mg/kg bw) ... . ... The mean plasma elimination halflives of MEHP were 3.9, 3.1 and 2.8 hours, respectively for 25, 40 and 60 days old /Sprague-Dawley/ rats. ... Two healthy male volunteers (47 and 34 years old) received 30 mg DEHP (> 99% pure) as a single dose or 10 mg/day of DEHP for 4 days ... A urinary elimination half-life of about 12 hours was estimated. ... For more Biological Half-Life (Complete) data for BIS(2-ETHYLHEXYL) PHTHALATE (9 total), please visit the HSDB record page. |
| Toxicity/Toxicokinetics |
Toxicity Summary IDENTIFICATION AND USE: Di(2-ethylhexyl)phthalate (DEHP) is a colorless, oily liquid. Plastics may contain from 1 to 40% DEHP by weight and are used in consumer products such as imitation leather, rainwear, footwear, upholstery, flooring, wire and cable, tablecloths, shower curtains, food packaging materials and children's toys. DEHP is also used as a hydraulic fluid and as a dielectric fluid (a non-conductor of electric current) in electrical capacitors, a detector for leaks in respirators. DEHP is not registered for current use in the U.S., but approved pesticide uses may change periodically and so federal, state and local authorities must be consulted for currently approved uses. HUMAN EXPOSURE AND TOXICITY: DEHP has been found in various types of food, such as fish, shellfish, eggs and cheese. Blood transfusions and other medical treatment using plastic devices may lead to involuntary human exposure to DEHP. Available data on oral administration indicate that DEHP is hydrolyzed in the gut by pancreatic lipase. The metabolites formed, i.e., mono(2-ethylhexyl)phthalate and 2-ethyl hexanol, are rapidly absorbed. Mono-2-ethylhexyl phthalate was detected in human teeth. When administered orally, DEHP is extensively hydrolyzed in the gut in certain animals, e.g., rats, and is mainly distributed as monoethylhexyl phthalate. However, hydrolysis occurs to a much lesser extent in primates and humans. Several further metabolites have been identified, omega- and omega-1-oxidation being the major metabolic pathways. DEHP metabolism shows considerable species differences, e.g., the omega-oxidation pathway is less extensive in humans than in rats. Bile and urine are the major excretory pathways. DEHP metabolites do not produce peroxisome proliferation in cultured human hepatocytes. Only very limited information is available on the effects of DEHP on humans. Mild gastric disturbances, but no other deleterious effects, were reported for two subjects. Adolescents exposed to significant quantities of DEHP as neonates showed no significant adverse effects on their physical growth and pubertal maturity. Thyroid, liver, renal, and male and female gonadal functions tested were within normal range for age and sex distribution. ANIMAL STUDIES: Hepatomegaly and increased relative kidney weights have been observed in treated animals in long term studies, also hypertrophic cells in the anterior pituitary. Several studies have shown testicular atrophy. Younger rats seem to be more susceptible than older ones, and rats and mice seem to be more sensitive than marmosets and hamsters. Reversibility of the atrophy has been observed. DEHP, as well as monoethylhexyl phthalate, shows teratogenic properties. Tests for mutagenicity and related end points have been negative in most studies. DEHP may induce cellular transformation, and it has been shown to be carcinogenic in rats and in mice. There was a dose-related increase in hepatocellular tumors in both sexes of both species. The induction of hepatic peroxisome proliferation and cell replication is strongly associated with the liver carcinogenic effects of certain non-genotoxic carcinogens including DEHP. However, marked differences have been observed among animal species with respect to DEHP-induced peroxisome proliferation. ECOTOXICITY STUDIES: Although few relevant studies have been reported, the acute toxicity of DEHP to algae, plants, and birds appears to be low. Monoethylhexylphthalate (MEHP), one of the major metabolites of DEHP, induces peroxisome proliferation by activating peroxisome proliferator activated receptors. This is believed to increase production of hydrogen peroxide by peroxisomes and enhance cell proliferation, leading to hepatotoxic and carcinogenic effects. MEHP is also believed to exhibit testicular toxicity by targeting and damaging the Sertoli cells. DEHP may act as an antiandrogen during a critical stage of reproductive tract differentiation by reducing testosterone in fetal males, hindering development. (L181, A106) Toxicity Data LD50: 33.9 g/kg (Oral, Rabbit) (T33) LD50: 10 g/kg (Dermal, Guinea pig) (T33) LD50: 30.7 g/kg (Intraperitoneal, Rat) (T33) Interactions In studies of the effects of DEHP ingestion on the metabolism of ethanol, there was a distinct difference between the action of single doses of 1,500-7,500 mg/kg DEHP and the same doses given over a 7-day period ... . The single dose appeared to decrease the metabolism of intraperitoneal ethanol, given 18 hours after DEHP, as reflected by an increase in the ethanol-induced sleeping time of the exposed rats and inhibition of hepatic alcohol dehydrogenase activity. On the other hand, when DEHP was given for 7 days before the ethanol, the ethanol-induced sleeping time was decreased and the activities of both alcohol and aldehyde dehydrogenase were increased. This indicates the changes in sleeping time were the result of more rapid metabolic removal of the alcohol from the system in the rats treated with repeated doses of DEHP and slower metabolism in the rats given one dose. ... One hypothesis is that altered zinc homeostasis is a cause of teratogenicity following DEHP exposure. On GD 9 (9 days post-coitus), CD-1 mice were given corn oil (vehicle) or DEHP 800 mg/kg bw by gavage. ... Maternal liver expression of metallothionein (MT)-I and MT-Il, enzymes that sequester zinc in liver and thus lower blood levels, were increased at 3.0-4.5 hours following DEHP exposure and then began returning to baseline levels at 6 hours following exposure. Maternal liver expression of zinc transporter-1 (ZnT-1), a transmembrane protein involved in zinc efflux, was not affected by DEHP exposure. Exposure to DEHP resulted in a down-regulation of MT-I, MT-Il, and ZnT-1 expression in embryonic brain from 3 to 6 hours following exposure. There was no effect on visceral yolk sac. A dose-response study was conducted in which pregnant mice were gavaged on GD 9 with 0, 50, 200, or 800 mg DEHP/kg bw. Dams were killed, and maternal liver and embryonic brains were collected at 3 hours following exposure. ... Up-regulation of MT-I ... in maternal liver reached statistical significance at 200 mg/kg bw/day DEHP ... /and/ MT-Il ... at 800 mg/kg bw. ... In embryonic brain, reductions in MT-I and ZnT-1 were significant at 200 mg/kg bw, and reductions in MT-Il were significant at 50 mg/kg bw. ... /It was/ concluded that exposure of dams to DEHP during periods of organogenesis can alter the expression of key fetal enzymes involved in zinc homeostasis. ... Four-week-old /F344 rats/ ... were stimulated with diethyistilbestrol or with pregnant mare serum gonadotropin (PMSG) following which ovaries were removed and granulosa cells harvested. Cells were cultured in the presence of 500 nM testosterone and 200 ng/mL FSH. MEHP ... was added to cultures /for 48 hr/ ... A comparison with other phthalate monoesters showed a decrease in estradiol in the medium (controlled for protein content) with MEHP 100 or 200 uM (27.8 or 55.6 mg/L) but not with comparable molar concentrations of monomethyl, -ethyl, -propyl, -butyl, -pentyl, or -hexyl phthalate. Monopentyl phthalate was associated with a decrease in estradiol production at 400 uM. mRNA for aromatase was estimated in media after culture with MEHP 0, 25, 50, or 100 uM (0, 7.0, 13.9, or 27.8 mg/L). Graphically, there appeared to be a concentration-dependent decrease in estradiol concentration and in aromatase mRNA; pair-wise comparisons with control were statistically significant for the 100 uM concentration for estradiol and for the 50 and 100 uM concentrations for aromatase mRNA. The peroxisome proliferator Wy-14,643 also decreased estradiol and aromatase mRNA. Cholesterol side-chain cleavage enzyme was not altered by MEHP ... . Aromatase protein was decreased by MEHP at concentrations of 100 and 200 uM (27.8 and 55.6 mg/L). In a final experiment, granulosa cells were incubated for 48 hours with MEHP 0 or 200 uM (0 or 56 mg/L) and 8-bromo-cyclic adenosine monophosphate (8-Br-cAMP) added for the last 24 hours. mRNA for aromatase and cholesterol side-chain cleavage enzyme and medium progesterone levels were increased by 8-Br-cAMP in the absence of MEHP. In the presence of MEHP, mRNA for aromatase and medium estradiol levels were suppressed, but there was no suppression of P450 side-chain cleavage enzyme mRNA or progesterone. ... The results /were interpreted/ as consistent with transcriptional suppression of aromatase by MEHP independent of the FSH-cAMP pathway. ... A peroxisome proliferator-activated receptor (PPAR) pathway /was proposed/ as a candidate mechanism for MEHP suppression of granulosa cell steroidogenic function. /MEHP/ ... Granulosa cells were harvested from 4-week-old Fisher rats 24 hours after injection of pregnant mare serum gonadotropin (PMSG). Cells were cultured for 48 hours with 500 nM testosterone and 200 ng/mL FSH with or without MEHP ... 50 uM (13.9 mg/L). ... MEHP in culture reduced aromatase mRNA by >40% compared to control. The addition of a peroxisome proliferator-activated receptor (PPAR)-gamma antagonist partially reversed the decrease in aromatase mRNA. PPAR-alpha and gamma agonists reduced aromatase mRNA to an extent similar to that after treatment with MEHP. To test the hypothesis that MEHP activated PPAR-gamma plus activated retinoic acid X receptor (RXR) results in aromatase suppression mediated by the PPAR-gamma:RXR heterodimer, cells were treated with MEHP plus RXR or RAR ligands. All treatments decreased aromatase, with significant additional suppression by MEHP when it was added with 9-cis-retinoic acid. To demonstrate that MEHP activity could be mediated through PPAR-alpha, MEHP treatment was shown to increase mRNA for 17 beta-hydroxysteroid dehydrogenase IV, which is inducible by PPAR-alpha. The addition of a PPAR-gamma antagonist did not alter the MEHP induction of 17 beta-hydroxysteroid dehydrogenase IV, suggesting MEHP activation of the alpha-isoform of PPAR. Both MEHP and a selective PPAR-alpha agonist, but not a selective PPAR-gamma agonist, increased the expression of Ah receptor, CYP1B1, and epoxide hydrolase. Cholesterol side-chain cleavage enzyme was not induced by MEHP or by either PPAR isoform agonist. Heart-type fatty acid-binding protein (H-FABP) was induced by MEHP and by each specific PPAR isoform agonist. ... /It was/ concluded that MEHP effects on granulosa cell gene expression, which would serve to decrease estrogen production, were mediated by both PPAR pathways. /MEHP/ For more Interactions (Complete) data for BIS(2-ETHYLHEXYL) PHTHALATE (21 total), please visit the HSDB record page. Non-Human Toxicity Values LD50 Rat oral >25 g/kg LD50 Rat iv 250 mg/kg LD50 Mouse oral >30 g/kg LD50 Mouse ip 14 g/kg For more Non-Human Toxicity Values (Complete) data for BIS(2-ETHYLHEXYL) PHTHALATE (10 total), please visit the HSDB record page. |
| References |
[1]. Impact of Deuterium Substitution on the Pharmacokinetics of Pharmaceuticals. Ann Pharmacother. 2019 Feb;53(2):211-216. |
| Additional Infomation |
Di(2-ethylhexyl) phthlate (DEHP) is a manufactured chemical that is commonly added to plastics to make them flexible. DEHP is a colorless liquid with almost no odor. DEHP is present in plastic products such as wall coverings, tablecloths, floor tiles, furniture upholstery, shower curtains, garden hoses, swimming pool liners, rainwear, baby pants, dolls, some toys, shoes, automobile upholstery and tops, packaging film and sheets, sheathing for wire and cable, medical tubing, and blood storage bags. Di(2-ethylhexyl)phthalate (DEHP) can cause cancer according to an independent committee of scientific and health experts. It can cause developmental toxicity and male reproductive toxicity according to NIOSH and the FDA. Di(2-ethylhexyl) phthalate is a colorless to pale yellow oily liquid. Nearly odorless. (USCG, 1999) Bis(2-ethylhexyl) phthalate is a phthalate ester that is the bis(2-ethylhexyl) ester of benzene-1,2-dicarboxylic acid. It has a role as an apoptosis inhibitor, an androstane receptor agonist and a plasticiser. It is a phthalate ester and a diester. Bis Bis(2-ethylhexyl) phthalate has been reported in Penicillium olsonii, Streptomyces, and other organisms with data available. Diethylhexylphthalate is a colorless, oily organic carcinogen with a slight odor. Bis(2-Ethylhexyl) Phthalate is mainly used as a plasticizer for fabricating flexible materials for many household products. Inhalation, digestion, and dermal contact are the primary routes of potential exposure, which was linked to increased incidence of hepatocellular carcinomas in animals. This substance is reasonably anticipated to be a human carcinogen. (NCI05) Di(2-ethylhexyl) phthlate (DEHP) is a manufactured chemical that is commonly added to plastics to make them flexible. DEHP exposure is generally low and not harmful, but increased exposures resulting from intravenous fluids delivered through plastic tubing or ingesting contaminated foods or water may have toxic effects. This is of particular concern since DEHP is known to leach into liquid that come in contact with DEHP containing plastic. (L181, L182) An ester of phthalic acid. It appears as a light-colored, odorless liquid and is used as a plasticizer for many resins and elastomers. Mechanism of Action ... A single dose of 1000 mg/kg bw MEHP (> 97% purity) in corn oil was administered by gavage to 5-week-old Sprague-Dawley rats, 28-day-old wild-type C57CL/6 mice, or 28-day-old gld mice. The gld mice express a dysfunctional fasL protein, which cannot bind to the fas receptor to initiate apoptosis. ... Following MEHP exposure, apoptosis was found to occur primarily in spermatocytes in both wild-type and gld mice. In wild-type mice, germ cell apoptosis was significantly increased from 6 to 48 hours following MEHP exposure. Apoptotic activity peaked between 12 and 24 hours with 5-fold increases compared to baseline levels. A significant ~2-fold increase in apoptosis compared to baseline levels was observed at 12 and 48 hours following MEHP exposure of gld mice. In both groups of mice, apoptotic activity returned to baseline levels by 96 hours following exposure. Western blot analyses revealed that fas expression significantly increased in wild-type mice (~ 3-fold) at 3 hours following MEHP exposure. There was no significant alteration in fas expression following MEHP exposure in gld mice. Expression of DR4, DR5, and DR6 proteins /which are fas-independent death receptors in the tumor necrosis factor (TNF) superfamily/ occurred in both wild-type and gld mice, but MEHP exposure did not increase expression in either strain. DR5 but not DR4 expression significantly increased in Sprague-Dawley rat testes (~1.5-fold) at 1.5 and 3 hours following MEHP exposure. Procaspase 8 cleavage products, downstream receptor-mediated signals of apoptotic pathways, were detected in testes of wild-type and gld mice, but expression was significantly increased only in gld mice at 6 hours following MEHP exposure. Electrophoretic mobility shift assays demonstrated that DNA binding of NFkappa3, a receptor-mediated downstream signal possibly involved in cell death or survival, was generally reduced in wild-type mice but upregulated in gld mice following MEHP exposure. ... /It was/ concluded that these findings demonstrate that germ-cell related death receptors and downstream signaling products appear to respond to MEHP-induced cell injury ... /MEHP/ Sprague-Dawley male rats were treated orally with 250, 500, or 750 mg/kg/d Di(2-ethylhexyl) phthalate (DEHP) for 28 days, while control rats were given corn oil. The levels of cell cycle regulators (pRb, cyclins, CDKs, and p21) and apoptosis-related proteins were analyzed by Western blot analysis. The role of PPAR-gamma (PPAR-gamma), class B scavenger receptor type 1 (SR-B1), and ERK1/2 was further studied to examine the signaling pathway for DEHP-induced apoptosis. Results showed that the levels of pRB, cyclin D, CDK2, cyclin E, and CDK4 were significantly lower in rats given 500 and 750 mg/kg/d DEHP, while levels of p21 were significantly higher in rat testes. Dose-dependent increases in PPAR-gamma and RXRalpha proteins were observed in testes after DEHP exposure, while there was a significant decrease in RXRgamma protein levels. In addition to PPAR-gamma, DEHP also significantly increased SR-B1 mRNA and phosphorylated ERK1/2 protein levels. Furthermore, DEHP treatment induced pro-caspase-3 and cleavage of its substrate protein, poly(ADP-ribose) polymerase (PARP), in a dose-dependent manner. Data suggest that DEHP exposure may induce the expresson of apoptosis-related genes in testes through induction of PPAR-gamma and activation of the ERK1/2 pathway. Global gene expression profiling combined with an evaluation of Gene Ontology (GO) and pathway mapping tools /was used/ ... for identifying the molecular pathways and processes affected /to examine/ ... the acute effects caused by the non-genotoxic carcinogen and peroxisome proliferator (PP) diethylhexylphthalate (DEHP) in the mouse liver as a model system. Consistent with what is known about the mode of action of DEHP, /the/ GO analysis of transcript profiling data revealed a striking overrepresentation of genes associated with the peroxisomal cellular component, together with genes involved in carboxylic acid and lipid metabolism. Furthermore ... gene expression changes associated with additional biological functions, including complement activation, hemostasis, the endoplasmic reticulum overload response, and circadian rhythm /were revealed/. Together, these data reveal potential new pathways of PP action and shed new light on the mechanisms by which non-genotoxic carcinogens control hepatocyte hypertrophy and proliferation. ... ... Peroxisome proliferator-activated receptor alpha (PPAR-alpha), the nuclear receptor, is a member of the steroid hormone receptor superfamily and binds to DNA as a heterodimer with the retinoid X receptor (RXR). Peroxisome proliferator response elements (PPREs) have been found in genes for both peroxisomal and microsomal fatty acid-oxidizing enzymes. ... The species differences /responding to peroxisome proliferators, eg DEHP/, particularly with respect to humans compared to rats and mice, can be potentially attributed to ... the level of expression and functional capability of PPAR-alpha, the presence or absence of active PPREs in the promoter region of specific genes, and other aspects of interaction with transcriptional regulatory proteins. ... Marked species differences in the expression of PPAR-alpha mRNA have been demonstrated between rodent and human liver, with the latter expressing 1-10% of the levels found in mouse or rat liver ... PPAR-alpha protein expression /in human livers/ contained less than 10% of the level in mice. ... In most human samples studied, it was found that PPREs are mainly bound by other competing proteins that may block peroxisome proliferator responsiveness. In addition, the low levels of PPAR-alpha protein detected in human liver were lower than those estimated from RNA analysis and this was explained by the finding that a significant fraction of PPAR-alpha mRNA is mis-spliced in human liver. ... The truncated PPAR-alpha mRNA accounted for 25-50% of total PPAR-alpha mRNA in 10 human liver samples, while no truncated PPAR-alpha mRNA was found in livers of rats and mice. The truncated human PPAR-alpha mRNA was expressed in vitro, where it was shown to (a) fail to bind to PPRE, a necessary step for gene activation and (b) interfere with gene activation by expressed full-length human PPAR-alpha, in part due to titration of coactivator CREB-binding protein, an additional element of transcriptional regulation. ... Differential species sensitivity to peroxisome proliferators could depend on gene-specific factors. In the case of peroxisomal acyl-coenzyme A oxidase, the promoter regions containing PPRE responsible for transcriptional activation of the rodent gene are not present in the promoter region of the human gene ... The absence of a significant response of human liver to induction of peroxisome proliferation and hepatocellular proliferation is explained by several aspects of PPAR-alpha-mediated regulation of gene expression. ... Overall, these findings indicate that the increased incidence of liver tumors in mice and rats treated with di(2-ethylhexyl) phthalate results from a mechanism that does not operate in humans. |
Solubility Data
| Solubility (In Vitro) | May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples |
| Solubility (In Vivo) |
Note: Listed below are some common formulations that may be used to formulate products with low water solubility (e.g. < 1 mg/mL), you may test these formulations using a minute amount of products to avoid loss of samples. Injection Formulations (e.g. IP/IV/IM/SC) Injection Formulation 1: DMSO : Tween 80: Saline = 10 : 5 : 85 (i.e. 100 μL DMSO stock solution → 50 μL Tween 80 → 850 μL Saline) *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH ₂ O to obtain a clear solution. Injection Formulation 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL DMSO → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Injection Formulation 3: DMSO : Corn oil = 10 : 90 (i.e. 100 μL DMSO → 900 μL Corn oil) Example: Take the Injection Formulation 3 (DMSO : Corn oil = 10 : 90) as an example, if 1 mL of 2.5 mg/mL working solution is to be prepared, you can take 100 μL 25 mg/mL DMSO stock solution and add to 900 μL corn oil, mix well to obtain a clear or suspension solution (2.5 mg/mL, ready for use in animals). Injection Formulation 4: DMSO : 20% SBE-β-CD in saline = 10 : 90 [i.e. 100 μL DMSO → 900 μL (20% SBE-β-CD in saline)] *Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Injection Formulation 5: 2-Hydroxypropyl-β-cyclodextrin : Saline = 50 : 50 (i.e. 500 μL 2-Hydroxypropyl-β-cyclodextrin → 500 μL Saline) Injection Formulation 6: DMSO : PEG300 : castor oil : Saline = 5 : 10 : 20 : 65 (i.e. 50 μL DMSO → 100 μLPEG300 → 200 μL castor oil → 650 μL Saline) Injection Formulation 7: Ethanol : Cremophor : Saline = 10: 10 : 80 (i.e. 100 μL Ethanol → 100 μL Cremophor → 800 μL Saline) Injection Formulation 8: Dissolve in Cremophor/Ethanol (50 : 50), then diluted by Saline Injection Formulation 9: EtOH : Corn oil = 10 : 90 (i.e. 100 μL EtOH → 900 μL Corn oil) Injection Formulation 10: EtOH : PEG300:Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL EtOH → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Oral Formulations Oral Formulation 1: Suspend in 0.5% CMC Na (carboxymethylcellulose sodium) Oral Formulation 2: Suspend in 0.5% Carboxymethyl cellulose Example: Take the Oral Formulation 1 (Suspend in 0.5% CMC Na) as an example, if 100 mL of 2.5 mg/mL working solution is to be prepared, you can first prepare 0.5% CMC Na solution by measuring 0.5 g CMC Na and dissolve it in 100 mL ddH2O to obtain a clear solution; then add 250 mg of the product to 100 mL 0.5% CMC Na solution, to make the suspension solution (2.5 mg/mL, ready for use in animals). Oral Formulation 3: Dissolved in PEG400 Oral Formulation 4: Suspend in 0.2% Carboxymethyl cellulose Oral Formulation 5: Dissolve in 0.25% Tween 80 and 0.5% Carboxymethyl cellulose Oral Formulation 6: Mixing with food powders Note: Please be aware that the above formulations are for reference only. InvivoChem strongly recommends customers to read literature methods/protocols carefully before determining which formulation you should use for in vivo studies, as different compounds have different solubility properties and have to be formulated differently. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.3321 mL | 11.6607 mL | 23.3214 mL | |
| 5 mM | 0.4664 mL | 2.3321 mL | 4.6643 mL | |
| 10 mM | 0.2332 mL | 1.1661 mL | 2.3321 mL |