Physicochemical Properties
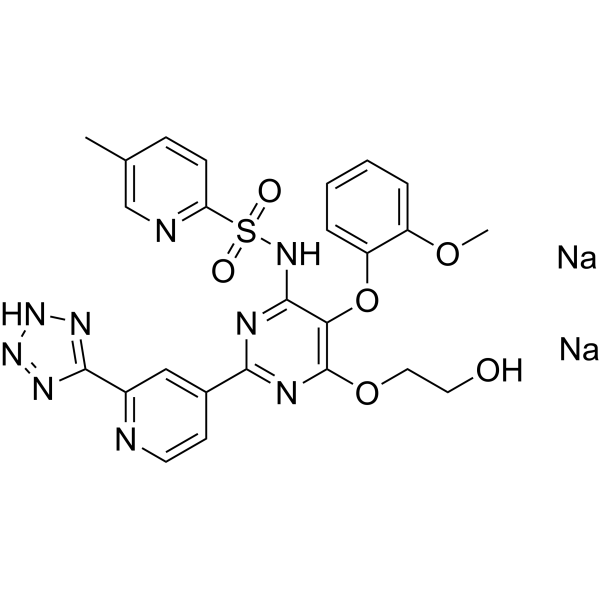
| Molecular Formula | C25H23N9NA2O6S |
| Molecular Weight | 623.55 |
| Exact Mass | 621.113 |
| Elemental Analysis | C, 48.31; H, 3.41; N, 20.28; Na, 7.40; O, 15.44; S, 5.16 |
| CAS # | 503271-02-1 |
| Related CAS # | 180384-56-9; 503271-02-1 (sodium) |
| PubChem CID | 51346597 |
| Appearance | Typically exists as solid at room temperature |
| LogP | 3.186 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 15 |
| Rotatable Bond Count | 11 |
| Heavy Atom Count | 43 |
| Complexity | 911 |
| Defined Atom Stereocenter Count | 0 |
| SMILES | S(C1C=CC(C)=CN=1)([N-]C1C(=C(N=C(C2C=CN=C(C3=NN=N[N-]3)C=2)N=1)OCCO)OC1C=CC=CC=1OC)(=O)=O.[Na+].[Na+] |
| InChi Key | PZNSONUYVNYXJZ-UHFFFAOYSA-N |
| InChi Code | InChI=1S/C25H21N9O6S.2Na/c1-15-7-8-20(27-14-15)41(36,37)32-24-21(40-19-6-4-3-5-18(19)38-2)25(39-12-11-35)29-22(28-24)16-9-10-26-17(13-16)23-30-33-34-31-23;;/h3-10,13-14,35H,11-12H2,1-2H3;;/q-2;2*+1 |
| Chemical Name | disodium;[6-(2-hydroxyethoxy)-5-(2-methoxyphenoxy)-2-[2-(1,2,3-triaza-4-azanidacyclopenta-2,5-dien-5-yl)pyridin-4-yl]pyrimidin-4-yl]-(5-methylpyridin-2-yl)sulfonylazanide |
| Synonyms | Ro 61-1790 disodium; VML 588 disodium; Clazosentan sodium; Clazosentan disodium salt; Clazosentan disodium; Clazosentan sodium [JAN]; Clazosentan disodium salt [MI]; 180384-56-9; AXV-034343; VML-588; Ro-61-1790; AXV-343434; Ro 61-1790; ACT-108475; AXV-034343 disodium |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | ETA/endothelin A receptor |
| ln Vitro | Clazosentan is a selective endothelin A receptor antagonist in development for the prevention and treatment of vasospasm postsubarachnoid hemorrhage. It is a substrate of organic anion-transporting polypeptide 1B1/1B3 based on preclinical data. The present data characterize clazosentan as a potent competitive antagonist of ET(A) receptor-mediated constriction of the cerebrovasculature by ET-1 and its precursor big ET-1. These functional data may also be used to define an in vitro profile of an ET receptor antagonist with a high probability of clinical efficacy. [3] |
| ln Vivo |
The pharmacokinetics of clazosentan are characterized by an intermediate clearance, a volume of distribution similar to that of the extracellular fluid volume, dose-proportional exposure, an elimination independent of drug-metabolizing enzymes, and a disposition mainly dependent on the hepatic uptake transporter organic anion transport polypeptide 1B1/1B3. In healthy subjects, clazosentan leads to an increase in ET-1 concentration and prevents the cardiac and renal effects mediated by infusion of ET-1. In patients, it significantly reduced the incidence of moderate or severe vasospasm as well as post-aSAH vasospasm-related morbidity and mortality. Clazosentan is well tolerated up to the expected therapeutic dose of 15 mg/h and, in aSAH patients, lung complications, hypotension, and anemia were adverse events more commonly reported following clazosentan than placebo. In summary, clazosentan has a pharmacokinetic, pharmacodynamic, and safety profile suitable to become a valuable asset in the armamentarium of therapeutic modalities to prevent aSAH-induced cerebral vasospasm. [1] Cerebral vasospasm and late cerebral ischemia (LCI) remain leading causes of mortality in patients experiencing a subarachnoid hemorrhage (SAH). This occurs typically 3 to 4 days after the initial bleeding and peaks at 5 to 7 days. The underlying pathophysiology is still poorly understood. Because SAH is associated with elevated levels of endothelin-1 (ET-1), focus has been on counteracting endothelin receptor activation with receptor antagonists like clazosentan, however, with poor outcome in clinical trials. We hypothesize that inhibition of intracellular transcription signaling will be an effective approach to prevent LCI. Here, we compare the effects of clazosentan versus the MEK1/2 blocker U0126 in a rat model of SAH. Although clazosentan directly inhibits the contractile responses in vivo to ET-1, it did not prevent SAH-induced upregulation of ET receptors in cerebral arteries and did not show a beneficial effect on neurologic outcome. U0126 had no vasomotor effect by itself but counteracts SAH-induced receptor upregulation in cerebral arteries and improved outcome after SAH. We suggest that because SAH induces elevated expression of several contractile receptor subtypes, it is not sufficient to block only one of these (ET receptors) but inhibition of transcriptional MEK1/2-mediated upregulation of several contractile receptors may be a viable way towards alleviating LCI. [2] This randomized, double-blind, two-period, cross-over study investigated the pharmacokinetics, safety, and tolerability of an intravenous infusion of clazosentan (15 mg/hour for 3 hours) after the intravenous administration of placebo or rifampin (600 mg/100 mL in 30 minutes). A total of 14 healthy male participants were enrolled resulting in 13 completers. Clazosentan exposure was three to four times higher after organic anion-transporting polypeptide 1B1/1B3 inhibition, as reflected by the geometric mean ratio (90% confidence interval) of area under the plasma concentration-time curve from zero to infinity: 3.88 (3.24-4.65). Clearance and volume of distribution decreased to a similar extent. Elimination half-life was not affected. A similar pattern but a higher incidence and frequency of adverse events were observed when clazosentan was given with rifampin than with placebo.[5] |
| Animal Protocol | Isometric force measurements were performed in rat basilar artery (BA) ring segments with (E+) and without (E-) endothelial function. Concentration effect curves (CECs) were constructed by cumulative application of ET-1 or big ET-1 in the absence or presence of clazosentan (10(-9), 10(-8), and 10(-7) M). The inhibitory potency of clazosentan was determined by the value of the affinity constant (pA2). The CECs for contraction induced by ET-1 and big ET-1 were shifted to the right in the presence of clazosentan in a parallel dose-dependent manner, which indicates competitive antagonism. The pA2 values for ET-1 were 7.8 (E+) and 8.6 (E-) and the corresponding values for big ET-1 were 8.6 (E+) and 8.3 (E-). [3] |
| References |
[1]. Clinical Pharmacology of Clazosentan, a Selective Endothelin A Receptor Antagonist for the Prevention and Treatment of aSAH-Related Cerebral Vasospasm. Front Pharmacol. 2021 Feb 4;11:628956. [2]. MEK1/2 inhibitor U0126 but not endothelin receptor antagonist clazosentan reduces upregulation of cerebrovascular contractile receptors and delayed cerebral ischemia, and improves outcome after subarachnoid hemorrhage in rats. J Cereb Blood Flow Metab. 2015 Feb;35(2):329-37. [3]. Cerebrovascular characterization of clazosentan, the first nonpeptide endothelin receptor antagonist clinically effective for the treatment of cerebral vasospasm. Part I: inhibitory effect on endothelin(A) receptor-mediated contraction. J Neurosurg. 2005 Jun;102(6):1101-7. [4]. IL-33 mediates antigen-induced cutaneous and articular hypernociception in mice. Proc Natl Acad Sci U S A. 2008 Feb 19;105(7):2723-8. [5]. Influence of Rifampin-Mediated Organic Anion-Transporting Polypeptide 1B1/1B3 Inhibition on the Pharmacokinetics of Clazosentan. Clin Transl Sci. 2019 Sep;12(5):440-444. |
| Additional Infomation |
CLAZOSENTAN is a small molecule drug with a maximum clinical trial phase of III (across all indications) and has 2 investigational indications. The central role of endothelin (ET)-1 in the development of cerebral vasospasm after subarachnoid hemorrhage is indicated by the successful treatment of this vasospasm in several animal models by using selective ET(A) receptor antagonists. Clazosentan is a selective ET(A) receptor antagonist that provides for the first time clinical proof that ET-1 is involved in the pathogenesis of cerebral vasospasm. The aim of the present investigation was, therefore, to define the pharmacological properties of clazosentan that affect ET(A) receptor-mediated contraction in the cerebrovasculature.[3] IL-33, a new member of the IL-1 family, signals through its receptor ST2 and induces T helper 2 (Th2) cytokine synthesis and mediates inflammatory response. We have investigated the role of IL-33 in antigen-induced hypernociception. Recombinant IL-33 induced cutaneous and articular mechanical hypernociception in a time- and dose-dependent manner. The hypernociception was inhibited by soluble (s) ST2 (a decoy receptor of IL-33), IL-1 receptor antagonist (IL-1ra), bosentan [a dual endothelin (ET)(A)/ET(B) receptor antagonist], clazosentan (an ET(A) receptor antagonist), or indomethacin (a cyclooxygenase inhibitor). IL-33 induced hypernociception in IL-18(-/-) mice but not in TNFR1(-/-) or IFNgamma(-/-) mice. The IL-33-induced hypernociception was not affected by blocking IL-15 or sympathetic amines (guanethidine). Furthermore, methylated BSA (mBSA)-induced cutaneous and articular mechanical hypernociception depended on TNFR1 and IFNgamma and was blocked by sST2, IL-1ra, bosentan, clazosentan, and indomethacin. mBSA also induced significant IL-33 and ST2 mRNA expression. Importantly, we showed that mBSA induced hypernociception via the IL-33 --> TNFalpha --> IL-1beta --> IFNgamma --> ET-1 --> PGE(2) signaling cascade. These results therefore demonstrate that IL-33 is a key mediator of immune inflammatory hypernociception normally associated with a Th1 type of response, revealing a hitherto unrecognized function of IL-33 in a key immune pharmacological pathway that may be amenable to therapeutic intervention.[4] |
Solubility Data
| Solubility (In Vitro) | May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples |
| Solubility (In Vivo) |
Note: Listed below are some common formulations that may be used to formulate products with low water solubility (e.g. < 1 mg/mL), you may test these formulations using a minute amount of products to avoid loss of samples. Injection Formulations (e.g. IP/IV/IM/SC) Injection Formulation 1: DMSO : Tween 80: Saline = 10 : 5 : 85 (i.e. 100 μL DMSO stock solution → 50 μL Tween 80 → 850 μL Saline) *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH ₂ O to obtain a clear solution. Injection Formulation 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL DMSO → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Injection Formulation 3: DMSO : Corn oil = 10 : 90 (i.e. 100 μL DMSO → 900 μL Corn oil) Example: Take the Injection Formulation 3 (DMSO : Corn oil = 10 : 90) as an example, if 1 mL of 2.5 mg/mL working solution is to be prepared, you can take 100 μL 25 mg/mL DMSO stock solution and add to 900 μL corn oil, mix well to obtain a clear or suspension solution (2.5 mg/mL, ready for use in animals). Injection Formulation 4: DMSO : 20% SBE-β-CD in saline = 10 : 90 [i.e. 100 μL DMSO → 900 μL (20% SBE-β-CD in saline)] *Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Injection Formulation 5: 2-Hydroxypropyl-β-cyclodextrin : Saline = 50 : 50 (i.e. 500 μL 2-Hydroxypropyl-β-cyclodextrin → 500 μL Saline) Injection Formulation 6: DMSO : PEG300 : castor oil : Saline = 5 : 10 : 20 : 65 (i.e. 50 μL DMSO → 100 μLPEG300 → 200 μL castor oil → 650 μL Saline) Injection Formulation 7: Ethanol : Cremophor : Saline = 10: 10 : 80 (i.e. 100 μL Ethanol → 100 μL Cremophor → 800 μL Saline) Injection Formulation 8: Dissolve in Cremophor/Ethanol (50 : 50), then diluted by Saline Injection Formulation 9: EtOH : Corn oil = 10 : 90 (i.e. 100 μL EtOH → 900 μL Corn oil) Injection Formulation 10: EtOH : PEG300:Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL EtOH → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Oral Formulations Oral Formulation 1: Suspend in 0.5% CMC Na (carboxymethylcellulose sodium) Oral Formulation 2: Suspend in 0.5% Carboxymethyl cellulose Example: Take the Oral Formulation 1 (Suspend in 0.5% CMC Na) as an example, if 100 mL of 2.5 mg/mL working solution is to be prepared, you can first prepare 0.5% CMC Na solution by measuring 0.5 g CMC Na and dissolve it in 100 mL ddH2O to obtain a clear solution; then add 250 mg of the product to 100 mL 0.5% CMC Na solution, to make the suspension solution (2.5 mg/mL, ready for use in animals). Oral Formulation 3: Dissolved in PEG400 Oral Formulation 4: Suspend in 0.2% Carboxymethyl cellulose Oral Formulation 5: Dissolve in 0.25% Tween 80 and 0.5% Carboxymethyl cellulose Oral Formulation 6: Mixing with food powders Note: Please be aware that the above formulations are for reference only. InvivoChem strongly recommends customers to read literature methods/protocols carefully before determining which formulation you should use for in vivo studies, as different compounds have different solubility properties and have to be formulated differently. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.6037 mL | 8.0186 mL | 16.0372 mL | |
| 5 mM | 0.3207 mL | 1.6037 mL | 3.2074 mL | |
| 10 mM | 0.1604 mL | 0.8019 mL | 1.6037 mL |