Physicochemical Properties
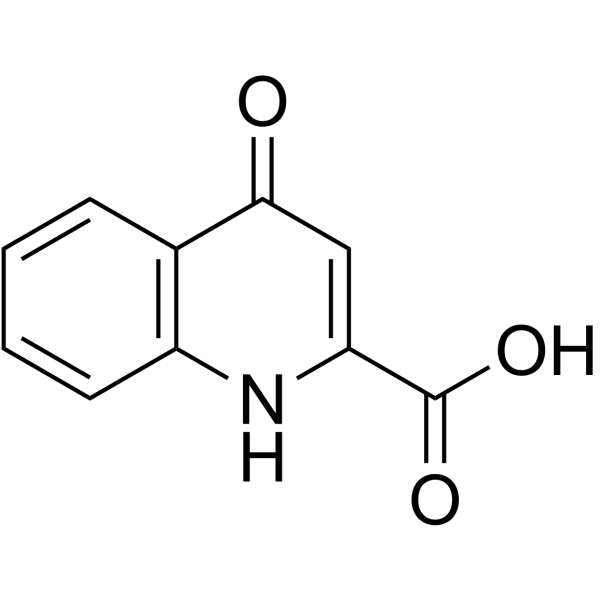
| Molecular Formula | C10H7NO3 |
| Molecular Weight | 189.17 |
| Exact Mass | 189.043 |
| CAS # | 13593-94-7 |
| PubChem CID | 3845 |
| Appearance | White to off-white solid powder |
| Density | 1.429g/cm3 |
| Boiling Point | 358.4ºC at 760mmHg |
| Melting Point | 280 °C |
| Flash Point | 170.5ºC |
| LogP | 1.226 |
| Hydrogen Bond Donor Count | 2 |
| Hydrogen Bond Acceptor Count | 4 |
| Rotatable Bond Count | 1 |
| Heavy Atom Count | 14 |
| Complexity | 309 |
| Defined Atom Stereocenter Count | 0 |
| InChi Key | HCZHHEIFKROPDY-UHFFFAOYSA-N |
| InChi Code | InChI=1S/C10H7NO3/c12-9-5-8(10(13)14)11-7-4-2-1-3-6(7)9/h1-5H,(H,11,12)(H,13,14) |
| Chemical Name | 4-oxo-1H-quinoline-2-carboxylic acid |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| ln Vitro | Transtorine demonstrates growth inhibitory efficacy with MIC values of 0.38, 0.5, and 0.45 mg/mL against Pseudomonas aeruginosa, Enterobacter cloacae, and Staphylococcus aureus, respectively[1]. |
| ADME/Pharmacokinetics |
Metabolism / Metabolites Uremic toxins tend to accumulate in the blood either through dietary excess or through poor filtration by the kidneys. Most uremic toxins are metabolic waste products and are normally excreted in the urine or feces. |
| References |
[1]. Transtorine, a new quinoline alkaloid from Ephedra transitoria. J Nat Prod. 1998 Feb;61(2):262-3. |
| Additional Infomation |
Kynurenic acid is a quinolinemonocarboxylic acid that is quinoline-2-carboxylic acid substituted by a hydroxy group at C-4. It has a role as a G-protein-coupled receptor agonist, a NMDA receptor antagonist, a nicotinic antagonist, a neuroprotective agent, a human metabolite and a Saccharomyces cerevisiae metabolite. It is a monohydroxyquinoline and a quinolinemonocarboxylic acid. It is a conjugate acid of a kynurenate. Kynurenic Acid is under investigation in clinical trial NCT02340325 (FS2 Safety and Tolerability Study in Healthy Volunteers). Kynurenic acid has been reported in Ephedra transitoria, Ephedra pachyclada, and other organisms with data available. Kynurenic acid is a uremic toxin. Uremic toxins can be subdivided into three major groups based upon their chemical and physical characteristics: 1) small, water-soluble, non-protein-bound compounds, such as urea; 2) small, lipid-soluble and/or protein-bound compounds, such as the phenols and 3) larger so-called middle-molecules, such as beta2-microglobulin. Chronic exposure of uremic toxins can lead to a number of conditions including renal damage, chronic kidney disease and cardiovascular disease. Kynurenic acid (KYNA) is a well-known endogenous antagonist of the glutamate ionotropic excitatory amino acid receptors N-methyl-D-aspartate (NMDA), alphaamino-3-hydroxy-5-methylisoxazole-4-propionic acid and kainate receptors and of the nicotine cholinergic subtype alpha 7 receptors. KYNA neuroprotective and anticonvulsive activities have been demonstrated in animal models of neurodegenerative diseases. Because of KYNA's neuromodulatory character, its involvement has been speculatively linked to the pathogenesis of a number of neurological conditions including those in the ageing process. Different patterns of abnormalities in various stages of KYNA metabolism in the CNS have been reported in Alzheimer's disease, Parkinson's disease and Huntington's disease. In HIV-1-infected patients and in patients with Lyme neuroborreliosis a marked rise of KYNA metabolism was seen. In the ageing process KYNA metabolism in the CNS of rats shows a characteristic pattern of changes throughout the life span. A marked increase of the KYNA content in the CNS occurs before the birth, followed by a dramatic decline on the day of birth. A low activity was seen during ontogenesis, and a slow and progressive enhancement occurs during maturation and ageing. This remarkable profile of KYNA metabolism alterations in the mammalian brain has been suggested to result from the development of the organisation of neuronal connections and synaptic plasticity, development of receptor recognition sites, maturation and ageing. There is significant evidence that KYNA can improve cognition and memory, but it has also been demonstrated that it interferes with working memory. Impairment of cognitive function in various neurodegenerative disorders is accompanied by profound reduction and/or elevation of KYNA metabolism. The view that enhancement of CNS KYNA levels could underlie cognitive decline is supported by the increased KYNA metabolism in Alzheimer's disease, by the increased KYNA metabolism in down's syndrome and the enhancement of KYNA function during the early stage of Huntington's disease. Kynurenic acid is the only endogenous N-methyl-D-aspartate (NMDA) receptor antagonist identified up to now, that mediates glutamatergic hypofunction. Schizophrenia is a disorder of dopaminergic neurotransmission, but modulation of the dopaminergic system by glutamatergic neurotransmission seems to play a key role. Despite the NMDA receptor antagonism, kynurenic acid also blocks, in lower doses, the nicotinergic acetycholine receptor, i.e., increased kynurenic acid levels can explain psychotic symptoms and cognitive deterioration. Kynurenic acid levels are described to be higher in the cerebrospinal fluid (CSF) and in critical central nervous system (CNS) regions of schizophrenics as compared to controls. (A3279, A3280). Kynurenic acid is a metabolite found in or produced by Saccharomyces cerevisiae. A broad-spectrum excitatory amino acid antagonist used as a research tool. |
Solubility Data
| Solubility (In Vivo) |
Note: Listed below are some common formulations that may be used to formulate products with low water solubility (e.g. < 1 mg/mL), you may test these formulations using a minute amount of products to avoid loss of samples. Injection Formulations (e.g. IP/IV/IM/SC) Injection Formulation 1: DMSO : Tween 80: Saline = 10 : 5 : 85 (i.e. 100 μL DMSO stock solution → 50 μL Tween 80 → 850 μL Saline) *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH ₂ O to obtain a clear solution. Injection Formulation 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL DMSO → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Injection Formulation 3: DMSO : Corn oil = 10 : 90 (i.e. 100 μL DMSO → 900 μL Corn oil) Example: Take the Injection Formulation 3 (DMSO : Corn oil = 10 : 90) as an example, if 1 mL of 2.5 mg/mL working solution is to be prepared, you can take 100 μL 25 mg/mL DMSO stock solution and add to 900 μL corn oil, mix well to obtain a clear or suspension solution (2.5 mg/mL, ready for use in animals). Injection Formulation 4: DMSO : 20% SBE-β-CD in saline = 10 : 90 [i.e. 100 μL DMSO → 900 μL (20% SBE-β-CD in saline)] *Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Injection Formulation 5: 2-Hydroxypropyl-β-cyclodextrin : Saline = 50 : 50 (i.e. 500 μL 2-Hydroxypropyl-β-cyclodextrin → 500 μL Saline) Injection Formulation 6: DMSO : PEG300 : castor oil : Saline = 5 : 10 : 20 : 65 (i.e. 50 μL DMSO → 100 μLPEG300 → 200 μL castor oil → 650 μL Saline) Injection Formulation 7: Ethanol : Cremophor : Saline = 10: 10 : 80 (i.e. 100 μL Ethanol → 100 μL Cremophor → 800 μL Saline) Injection Formulation 8: Dissolve in Cremophor/Ethanol (50 : 50), then diluted by Saline Injection Formulation 9: EtOH : Corn oil = 10 : 90 (i.e. 100 μL EtOH → 900 μL Corn oil) Injection Formulation 10: EtOH : PEG300:Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL EtOH → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Oral Formulations Oral Formulation 1: Suspend in 0.5% CMC Na (carboxymethylcellulose sodium) Oral Formulation 2: Suspend in 0.5% Carboxymethyl cellulose Example: Take the Oral Formulation 1 (Suspend in 0.5% CMC Na) as an example, if 100 mL of 2.5 mg/mL working solution is to be prepared, you can first prepare 0.5% CMC Na solution by measuring 0.5 g CMC Na and dissolve it in 100 mL ddH2O to obtain a clear solution; then add 250 mg of the product to 100 mL 0.5% CMC Na solution, to make the suspension solution (2.5 mg/mL, ready for use in animals). Oral Formulation 3: Dissolved in PEG400 Oral Formulation 4: Suspend in 0.2% Carboxymethyl cellulose Oral Formulation 5: Dissolve in 0.25% Tween 80 and 0.5% Carboxymethyl cellulose Oral Formulation 6: Mixing with food powders Note: Please be aware that the above formulations are for reference only. InvivoChem strongly recommends customers to read literature methods/protocols carefully before determining which formulation you should use for in vivo studies, as different compounds have different solubility properties and have to be formulated differently. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 5.2863 mL | 26.4313 mL | 52.8625 mL | |
| 5 mM | 1.0573 mL | 5.2863 mL | 10.5725 mL | |
| 10 mM | 0.5286 mL | 2.6431 mL | 5.2863 mL |