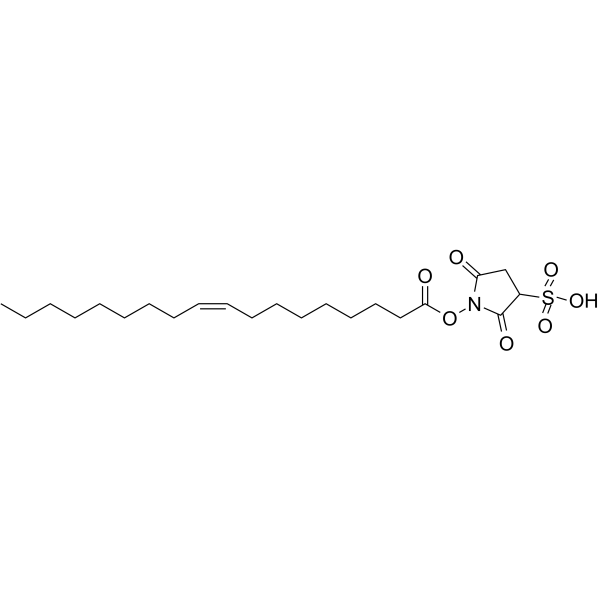
Sulfosuccinimidyl oleate (SSO) is a long chain fatty acid acting as an irreversible inhibitor of the fatty acid translocase CD36 with anti-inflammatory effects. When added at 200 M to adipocytes, it can 65% block the uptake of oleate, linoleate, or stearate. SSO is also a strong and permanent inhibitor of the mitochondrial respiratory chain.
Physicochemical Properties
| Molecular Formula | C22H37NO7S |
| Molecular Weight | 482.58648 |
| Exact Mass | 481.211 |
| Elemental Analysis | C, 54.87; H, 7.54; N, 2.91; Na, 4.77; O, 23.26; S, 6.66 |
| CAS # | 135661-44-8 |
| Related CAS # | Sulfosuccinimidyl oleate sodium;1212012-37-7 |
| PubChem CID | 90469841 |
| Appearance | Solid powder |
| Density | 1.19g/cm3 |
| Melting Point | 220-222ºC |
| Index of Refraction | 1.526 |
| LogP | 5.173 |
| Hydrogen Bond Donor Count | 0 |
| Hydrogen Bond Acceptor Count | 7 |
| Rotatable Bond Count | 18 |
| Heavy Atom Count | 32 |
| Complexity | 704 |
| Defined Atom Stereocenter Count | 0 |
| SMILES | O=S(C(C1)C(N(OC(CCCCCCC/C=C\CCCCCCCC)=O)C1=O)=O)(O)=O |
| InChi Key | IENDXPSKPJDQKO-UHFFFAOYSA-N |
| InChi Code | InChI=1S/C22H37NO7S.Na/c1-2-3-4-5-6-7-8-9-10-11-12-13-14-15-16-17-21(25)30-23-20(24)18-19(22(23)26)31(27,28)29;/h9-10,19H,2-8,11-18H2,1H3,(H,27,28,29) |
| Chemical Name | sodium;1-[(Z)-octadec-9-enoyl]oxy-2,5-dioxopyrrolidine-3-sulfonate |
| Synonyms | Sulfosuccinimidyl Oleate Sodium; sulfosuccinimidyl oleate; 135661-44-8; SCHEMBL2129565; CHEBI:183957; 1-(Oleoyloxy)-2,5-dioxopyrrolidine-3-sulfonic acid; SSO |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| ln Vitro |
Cell viability was not affected by sulfosuccinimidyl oleate (20 μM and 50 μM, 24 hours). Moderate exposure to 5 ng/mL IFNγ plus 100 ng/ml LPS dramatically decreased the viability of BV2 cells. Sulfosuccinimidyl oleate co-treatment stops the reduction in cell viability caused by LPS+IFNγ [1]. In BV2 cells, co-treatment with 50 μM sulfosuccinimidyl oleate for 24 hours dramatically decreased the production of NOS2 and COX-2 produced by LPS+IFNγ. The phosphorylated forms of p38 produced by LPS/IFNγ were significantly upregulated, as demonstrated by Western blot analysis. This overexpression was inhibited by co-treating the samples with 50 μM sulfosuccinimidyl oleate for a 24-hour period. [1].
sulfosuccinimidyl oleate (SSO) maintains the viability of BV2 microglia upon inflammatory stimuli [1] The ability of SSO to alter cell viability was first assessed with naïve BV2 cells or BV2 cells stimulated with 100 ng/ml LPS and 5 ng/ml IFNγ. Two concentrations of SSO (20 μM and 50 μM) were used. SSO alone did not alter the cellular viability as measured by the resazurin assay (Fig. 1a). Exposure to 100 ng/ml LPS + 5 ng/ml IFNγ modestly, yet significantly reduced the viability of the BV2 cells. Co-treatment with SSO prevented the LPS + IFNγ-induced reduction in the cell viability (Fig. 1a). In addition, LPS + IFNγ exposure induced a massive NO production in BV2 cells which was blocked by co-treatment with SSO at both concentrations (Fig. 1b). sulfosuccinimidyl oleate (SSO) downregulates LPS/IFNγ-induced inflammatory mediators in BV2 cells [1] Since 50 μM dose of SSO did not exert any toxicity, we chose to use SSO at the 50 μM concentration for further experiments. Next analyses focused on analyzing whether SSO exhibits anti-inflammatory properties in vitro in LPS + IFNγ-stimulated BV2 cells. Of the various cytokines analyzed, LPS + IFNγ promoted a massive increase in the secretion of IL-6 and TNF-α, which were significantly reduced by co-treatment with SSO (Fig. 2a, b). The levels of IL-10 were unaltered in all treatment groups (Fig. 2c). sulfosuccinimidyl oleate (SSO) rescues neurons from inflammation-induced death [1] We next assessed whether SSO is directly neuroprotective in cultured primary neurons exposed to glutamate-mediated excitotoxicity. Primary neurons were pre-treated with 50 μM SSO for 2 h followed by the exposure to 400 μM glutamate and 50 μM SSO for 24 h. SSO alone was not toxic to the neurons, yet it was unable to prevent glutamate-induced neuronal death (Fig. 5a). Since SSO was not able to rescue neuronal viability in pure neuronal cultures but has anti-inflammatory properties, we assessed whether SSO can prevent inflammation-induced neuronal death using primary neuron-BV2 co-cultures. The co-cultures were pre-treated with two concentrations of SSO (20 μM and 50 μM) followed by the exposure to 100 ng/ml LPS and 5 ng/ml IFNγ. Measurement of neuronal viability using peroxidase-ABTS kit showed that SSO alone was not causing any loss of MAP-2 immunoreactivity. Moreover, SSO dose-dependently prevented the LPS/IFNγ-induced neuronal death (Fig. 5b). To confirm these findings on primary microglia, we exposed a primary neuron-primary microglia co-culture model to 20 μM SSO, and similarly, 2-h SSO pre-treatment significantly prevented LPS + IFNγ-induced neuron death (Fig. 5c). |
| ln Vivo |
In male BALB/cABom mice in the pMCAo model, sulfosuccinimide oleate (50 mg/kg; administered as a single oral gavage) significantly reduced cortical defects compared with vehicle-treated controls. Blood infarct area. Additionally, 50 mg/kg of sulfosuccinimide oleate was suitable to see beneficial effects after stroke [1].
sulfosuccinimidyl oleate (SSO) treatment attenuates brain damage following ischemia [1] Based on our in vitro data, we then tested the therapeutic effect of SSO in a mouse model of pMCAo. We chose the dose of 50 mg/kg of SSO, which caused no adverse effect to the mice. The mice underwent MRI imaging at 3 days post-injury. Quantification of the lesion volumes revealed that orally administered SSO significantly reduced the cortical ischemic infarct size compared to vehicle-treated controls (Fig. 6). Peri-ischemic microgliosis but not astrogliosis was significantly reduced in sulfosuccinimidyl oleate (SSO)-treated mice [1] Ischemia-induced brain microgliosis was analyzed by immunohistochemical staining against Iba-1. As expected, we detected a significant upregulation of microgliosis in the peri-ischemic area of both the SSO-treated and control mice when compared to the corresponding area in the contralateral side at 3 days post-stroke (Fig. 7a). However, the extent of Iba-1 immunoreactivity in the peri-ischemic area of SSO-treated mice was significantly reduced compared to their vehicle-treated counterparts (Fig. 7a). Ischemia induced significant upregulation of GFAP immunoreactivity in the peri-ischemic area compared to the contralateral side, yet SSO failed to reduce stroke-induced increased GFAP immunoreactivity (Fig. 7b). sulfosuccinimidyl oleate (SSO)-treated mice showed reduced expression of COX-2 and increased expression of HO-1 in the peri-ischemic area [1] Due to the ability of SSO to reduce the expression of COX-2 in vitro, we analyzed the extent of COX-2 immunoreactivity in the peri-ischemic area of the stroked animals at 3 days post-stroke. pMCAo induced a significant upregulation in COX-2 immunoreactivity in the peri-ischemic area (Fig. 8a). SSO-treated animals showed a reduced extent of COX-2 expression compared to vehicle-treated controls (Fig. 8a). To evaluate the cell types expressing COX-2, we carried out immunohistological double stainings with COX-2 and microglial/macrophage marker CD45, neuronal marker NeuN, and astrocytic marker GFAP. The double stainings revealed that COX-2 immunoreactivity was mainly localized in microglia/macrophages and neurons but not in astrocytes (Fig. 8f). To evaluate the impact of SSO to induce antioxidant response, we carried out a staining against HO-1 and detected a significant upregulation in HO-1 in the peri-ischemic area in the SSO-treated animals when compared to vehicle-treated controls (Fig. 8g). Double stainings of HO-1 with CD45, NeuN, and GFAP revealed colocalization similar to COX-2, HO-1 was mainly expressed in microglia/macrophages and neurons, but not in astrocytes (Fig. 8l). |
| Cell Assay |
Western Blot Analysis[1] Cell Types: BV2 Cell Tested Concentrations: 50 μM Incubation Duration: 24 hrs (hours) Experimental Results: NOS2, COX-2 and P-p38/T-p38 levels were Dramatically increased. Measurement of nitric oxide production and cell viability assay [1] Nitric oxide (NO) production was assessed in the culture media by using Griess assay 24 h after LPS/IFNγ stimulation and sulfosuccinimidyl oleate (SSO) treatment. Fifty microliter of culture supernatant was incubated with an equal volume of Griess reagent for 10 min at room temperature (RT), and the optical density was measured at 544 nm using Victor 2.0 plate reader. Cell viability was measured using resazurin assay 24 h after exposure. Briefly, cells were incubated with 10 μM resazurin (Sigma-Aldrich) diluted in culture media for 2 h at 37 °C. The absorbance was then quantified at 485 nm using Victor 2.0 plate reader. CBA assay [1] Culture supernatants obtained 24 h after sulfosuccinimidyl oleate (SSO) treatment were used to determine the levels of interleukin-6 (IL-6), IL-10, monocyte chemoattractant protein 1 (MCP-1), TNF-α, IFN-γ, and IL-12p70 using a mouse anti-inflammatory cytometric bead array (CBA) kit). After staining, the samples were run on a FACS Calibur flow cytometer. The results were analyzed using FCAP array software |
| Animal Protocol |
Animal/Disease Models: 4-month-old male BALB/cABom mice, pMCAo model [1] Doses: 50 mg/kg Route of Administration: Single oral administration once Experimental Results:Reduce post-ischemic brain damage. The infarct area is diminished. Ischemia surgery and treatment with sulfosuccinimidyl oleate (SSO) [1] All animals underwent distal permanent occlusion of the middle cerebral artery (MCA) (pMCAo) as described previously. Briefly, mice were anesthetized with 5% isoflurane for induction and 2% isoflurane for maintenance (70% N2O/30% O2). The temperature of the mice was maintained at 36-5 ± 0.5 °C using a thermostatically controlled heating blanket connected to a rectal probe. The temporalis muscle was retracted to expose the skull in between the ear and the eye, and a small hole of approximately 1 mm was drilled at the site of the MCA. The dura was carefully removed to expose the MCA. The artery was then gently lifted up and cauterized using a thermocoagulator. After the procedure, the muscle was lifted back and the skin wound was sutured. The animals were then placed back to their home cages. SSO was emulsified in 0.5% methyl cellulose and administered once by single oral gavage at the dose of 50 mg/kg immediately after the surgery, when the mice had retained their consciousness. The administration routes for SSO in vivo have been described previously. In addition, we performed a dose-response study and found that SSO at 50 mg/kg was suitable to see a beneficial effect after stroke. There was no mortality in this study. |
| References |
[1]. Sulfosuccinimidyl oleate sodium is neuroprotective and alleviates stroke-induced neuroinflammation. J Neuroinflammation. 2017 Dec 4;14(1):237. [2]. Succinimidyl oleate, established inhibitor of CD36/FAT translocase inhibits complex III of mitochondrial respiratory chain. Biochem Biophys Res Commun. 2010 Jan 15;391(3):1348-51. |
| Additional Infomation |
Background: Ischemic stroke is one of the main causes of death and disability worldwide. It is caused by the cessation of cerebral blood flow resulting in the insufficient delivery of glucose and oxygen to the neural tissue. The inflammatory response initiated by ischemic stroke in order to restore tissue homeostasis in the acute phase of stroke contributes to delayed brain damage.
Methods: By using in vitro models of neuroinflammation and in vivo model of permanent middle cerebral artery occlusion, we demonstrate the neuroprotective and anti-inflammatory effects of sulfosuccinimidyl oleate sodium (SSO). Results: SSO significantly reduced the lipopolysaccharide/interferon-γ-induced production of nitric oxide, interleukin-6 and tumor necrosis factor-α, and the protein levels of inflammatory enzymes including nitric oxide synthase 2, cyclooxygenase-2 (COX-2), and p38 mitogen-activated protein kinase (MAPK) in microglia, without causing cell toxicity. Although SSO failed to directly alleviate glutamate-induced excitotoxicity in murine cortical neurons, it prevented inflammation-induced neuronal death in microglia-neuron co-cultures. Importantly, oral administration of SSO in Balb/c mice subjected to permanent occlusion of the middle cerebral artery reduced microglial activation in the peri-ischemic area and attenuated brain damage. This in vivo neuroprotective effect of SSO was associated with a reduction in the COX-2 and heme oxygenase-1 immunoreactivities. Conclusions: Our results suggest that SSO is an anti-inflammatory and a possible therapeutic candidate in diseases such as stroke where inflammation is a central hallmark.[1] The functional role of CD36 protein detected in mitochondrial fractions in long chain fatty acid (LCFA) oxidation is unclear due to conflicting results obtained in Cd36 knockout mice and experiments using sulfo-N-succinimidyl oleate (SSO) for inhibition of CD36 mediated LCFA transport. We investigated effect of SSO on mitochondrial respiration and found that SSO substantially inhibits not only LCFA oxidation, but also oxidation of flavoprotein- and NADH-dependent substrates and generation of mitochondrial membrane potential. Experiments in rat liver, heart and kidney mitochondria demonstrated a direct effect on mitochondrial respiratory chain with the most pronounced inhibition of the complex III (IC(50) 4microM SSO). The results presented here show that SSO is a potent and irreversible inhibitor of mitochondrial respiratory chain.[2] |
Solubility Data
| Solubility (In Vitro) | May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples |
| Solubility (In Vivo) |
Note: Listed below are some common formulations that may be used to formulate products with low water solubility (e.g. < 1 mg/mL), you may test these formulations using a minute amount of products to avoid loss of samples. Injection Formulations (e.g. IP/IV/IM/SC) Injection Formulation 1: DMSO : Tween 80: Saline = 10 : 5 : 85 (i.e. 100 μL DMSO stock solution → 50 μL Tween 80 → 850 μL Saline) *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH ₂ O to obtain a clear solution. Injection Formulation 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL DMSO → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Injection Formulation 3: DMSO : Corn oil = 10 : 90 (i.e. 100 μL DMSO → 900 μL Corn oil) Example: Take the Injection Formulation 3 (DMSO : Corn oil = 10 : 90) as an example, if 1 mL of 2.5 mg/mL working solution is to be prepared, you can take 100 μL 25 mg/mL DMSO stock solution and add to 900 μL corn oil, mix well to obtain a clear or suspension solution (2.5 mg/mL, ready for use in animals). Injection Formulation 4: DMSO : 20% SBE-β-CD in saline = 10 : 90 [i.e. 100 μL DMSO → 900 μL (20% SBE-β-CD in saline)] *Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Injection Formulation 5: 2-Hydroxypropyl-β-cyclodextrin : Saline = 50 : 50 (i.e. 500 μL 2-Hydroxypropyl-β-cyclodextrin → 500 μL Saline) Injection Formulation 6: DMSO : PEG300 : castor oil : Saline = 5 : 10 : 20 : 65 (i.e. 50 μL DMSO → 100 μLPEG300 → 200 μL castor oil → 650 μL Saline) Injection Formulation 7: Ethanol : Cremophor : Saline = 10: 10 : 80 (i.e. 100 μL Ethanol → 100 μL Cremophor → 800 μL Saline) Injection Formulation 8: Dissolve in Cremophor/Ethanol (50 : 50), then diluted by Saline Injection Formulation 9: EtOH : Corn oil = 10 : 90 (i.e. 100 μL EtOH → 900 μL Corn oil) Injection Formulation 10: EtOH : PEG300:Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL EtOH → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Oral Formulations Oral Formulation 1: Suspend in 0.5% CMC Na (carboxymethylcellulose sodium) Oral Formulation 2: Suspend in 0.5% Carboxymethyl cellulose Example: Take the Oral Formulation 1 (Suspend in 0.5% CMC Na) as an example, if 100 mL of 2.5 mg/mL working solution is to be prepared, you can first prepare 0.5% CMC Na solution by measuring 0.5 g CMC Na and dissolve it in 100 mL ddH2O to obtain a clear solution; then add 250 mg of the product to 100 mL 0.5% CMC Na solution, to make the suspension solution (2.5 mg/mL, ready for use in animals). Oral Formulation 3: Dissolved in PEG400 Oral Formulation 4: Suspend in 0.2% Carboxymethyl cellulose Oral Formulation 5: Dissolve in 0.25% Tween 80 and 0.5% Carboxymethyl cellulose Oral Formulation 6: Mixing with food powders Note: Please be aware that the above formulations are for reference only. InvivoChem strongly recommends customers to read literature methods/protocols carefully before determining which formulation you should use for in vivo studies, as different compounds have different solubility properties and have to be formulated differently. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.0722 mL | 10.3608 mL | 20.7215 mL | |
| 5 mM | 0.4144 mL | 2.0722 mL | 4.1443 mL | |
| 10 mM | 0.2072 mL | 1.0361 mL | 2.0722 mL |