Ribociclib HCl (formerly also known as LEE-011, NVP-LEE011; Kisqali), the hydrochloride salt of Ribociclib, is an orally bioavailable CDK4/6 (cyclin-dependent kinase) inhibitor (IC50s = 10 nM and 39 nM) approved in March 2017 by FDA to treat postmenopausal women with a type of advanced breast cancer. Ribociclib works by reducing FOXM1 and phosphorylated RB.
Physicochemical Properties
| Molecular Formula | C23H31CLN8O |
| Molecular Weight | 471.01 |
| Exact Mass | 470.231 |
| Elemental Analysis | C, 58.65; H, 6.63; Cl, 7.53; N, 23.79; O, 3.40 |
| CAS # | 1211443-80-9 |
| Related CAS # | Ribociclib;1211441-98-3;Ribociclib-d6 hydrochloride;Ribociclib succinate;1374639-75-4;Ribociclib succinate hydrate;1374639-79-8 |
| PubChem CID | 67242274 |
| Appearance | Yellow solid powder |
| LogP | 4.065 |
| Hydrogen Bond Donor Count | 3 |
| Hydrogen Bond Acceptor Count | 7 |
| Rotatable Bond Count | 5 |
| Heavy Atom Count | 33 |
| Complexity | 636 |
| Defined Atom Stereocenter Count | 0 |
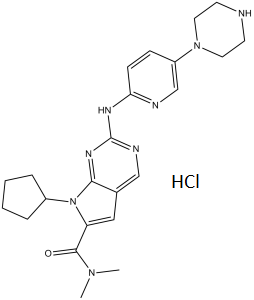
| SMILES | Cl[H].O=C(C1=C([H])C2=C([H])N=C(N([H])C3C([H])=C([H])C(=C([H])N=3)N3C([H])([H])C([H])([H])N([H])C([H])([H])C3([H])[H])N=C2N1C1([H])C([H])([H])C([H])([H])C([H])([H])C1([H])[H])N(C([H])([H])[H])C([H])([H])[H] |
| InChi Key | JZRSIQPIKASMEV-UHFFFAOYSA-N |
| InChi Code | InChI=1S/C23H30N8O.ClH/c1-29(2)22(32)19-13-16-14-26-23(28-21(16)31(19)17-5-3-4-6-17)27-20-8-7-18(15-25-20)30-11-9-24-10-12-30;/h7-8,13-15,17,24H,3-6,9-12H2,1-2H3,(H,25,26,27,28);1H |
| Chemical Name | 7-cyclopentyl-N,N-dimethyl-2-[(5-piperazin-1-ylpyridin-2-yl)amino]pyrrolo[2,3-d]pyrimidine-6-carboxamide;hydrochloride |
| Synonyms | NVP-LEE011; LEE011; LEE-011; LEE011 HCl; LEE-011 HCl; LEE 011 HCl; trade name: Kisqali; Ribociclib hydrochloride; LEE011 hydrochloride; Ribociclib HCl; LEE011 (hydrochloride); 7-Cyclopentyl-N,N-dimethyl-2-((5-(piperazin-1-yl)pyridin-2-yl)amino)-7H-pyrrolo[2,3-d]pyrimidine-6-carboxamide hydrochloride; 63YF7YKW7E; 7-cyclopentyl-N,N-dimethyl-2-[(5-piperazin-1-ylpyridin-2-yl)amino]pyrrolo[2,3-d]pyrimidine-6-carboxamide;hydrochloride; |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month Note: Please store this product in a sealed and protected environment, avoid exposure to moisture. |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | CDK4 (IC50 = 10 nM); CDK6 (IC50 = 39 nM) |
| ln Vitro | Treating a panel of 17 neuroblastoma cell lines with Ribociclib (LEE011) across a four-log dose range (10 to 10,000 nM). In 12 of the 17 neuroblastoma cell lines that were studied, treatment with ribociclib dramatically reduces substrate adherent growth in comparison to the control (mean IC50=306±68 nM, taking only sensitive lines into consideration; sensitivity is defined as an IC50 of less than 1 μM). After being treated with ribofloxacilb, two neuroblastoma cell lines (IMR5 and BE2C) that have been shown to be sensitive to CDK4/6 inhibition accumulate cells in the G0/G1 phase of the cell cycle in a dose-dependent manner. At concentrations of 100 nM (p=0.007) and 250 nM (p=0.01), respectively, of Ribociclib, this G0/G1 arrest becomes significant[2]. |
| ln Vivo |
Ribociclib (LEE011; 200 mg/kg) or a vehicle control is administered once daily for 21 days to CB17 immunodeficient mice carrying BE2C, NB-1643 (MYCN amplified, sensitive in vitro), or EBC1 (non-amplified, resistant in vitro) xenografts. Since none of the xenograft models exhibit weight loss or other toxicity indicators, this dosage strategy is well tolerated. During the course of the 21-day treatment period, mice carrying either the BE2C or 1643 xenografts (both, p<0.0001) showed a significant delay in tumor growth, which did not resume after treatment[2]. CDK4/6 inhibition by Ribociclib (LEE011) causes tumor growth delay in vivo [2] Given the observed differential sensitivity of neuroblastoma cell lines to CDK4/6 inhibition, we assayed for in vivo efficacy using neuroblastoma cell-line derived xenografts representing the extremes of in vitro sensitivity. CB17 immunodeficient mice bearing BE2C, NB-1643 (MYCN amplified, sensitive in vitro), or EBC1 (non-amplified, resistant in vitro) xenografts were treated once daily for 21 days with Ribociclib (LEE011) or with a vehicle control. This dosing strategy was well tolerated, as no weight loss or other signs of toxicity were observed in any of the xenograft models. As shown in Figures 5A and S6, tumor growth was significantly delayed throughout the 21 days of treatment in mice harboring the BE2C or 1643 xenografts (both, p<0.0001), although growth resumed post-treatment (data not shown). By contrast, as anticipated by the in vitro data, tumor growth suppression was less robust in the EBC1 xenograft model (p=0.51). Assessment of the Ki67 proliferation marker by immunohistochemistry confirmed that proliferation was impaired only in the BE2C and 1643 xenograft models, as tumors resected from separate cohorts of BE2C or 1643 xenografted mice demonstrated comparatively weaker staining following 7 days of treatment with Ribociclib (LEE011) than with the vehicle control, while no Ki67 staining differences were observed in the EBC1 xenografts (Figure 5B). Phosphorylation of RB was also substantially diminished in the BE2C and 1643 xenografts, while only a minimal decrease was detected in the EBC1 model (Figures 5B and 5C) [2]. |
| Enzyme Assay | Ribociclib, a powerful, oral, and highly selective inhibitor of CDK4/6 (cyclin-dependent kinase), with IC50s of 10 nM and 39 nM, respectively, was previously known as LEE011, NVP-LEE011; trade name: Kisqali. In March 2017, the FDA approved Ribociclib as a treatment for postmenopausal women who had an advanced form of breast cancer. Ribociclib works by reducing the levels of phosphorylated FOXM1 and RB. Out of 17 human neuroblastoma cell lines tested, 12 showed sensitivity to ribofacilb treatment (mean IC50=306±68 NM). By stopping the G0-G1 cell cycle, ribociclib treatment may significantly reduce the rate of cell proliferation. Treatment with LEE011 could markedly inhibit cell proliferation in 12 out of 17 human neuroblastoma-derived cell lines. |
| Cell Assay | In 35 mm plates, cells are grown for 24 hours, then treated with 500 nM Ribociclib for 6 days. The cells are then fixed, and overnight staining is done. Then, using an Axio Observer D.1 phase contrast microscope, cells are imaged for SA-β-gal. By counting the number of positive cells in three different microscope frames and normalizing to the control, one can calculate the percentage of SA-β-gal positive cells. In order to evaluate apoptotic activity, cells are treated with Ribociclib, plated in triplicate in 96-well plates, and then 16 hours later, caspase 3/7 activation is measured 16 hours after Caspase-Glo 3/7 treatment. As a positive control, SN-38-treated cells are employed[2]. |
| Animal Protocol | Mice: The xenografts derived from BE2C, NB-1643, or EBC1 cell lines are subcutaneously implanted into the right flank of CB17 SCID-/-mice. Then, for a total of 21 days, animals with engrafted tumors measuring 200–600 mm3 are randomly assigned to receive oral treatment with 200 mg/kg Ribociclib in 0.5% methylcellulose (n = 10) or vehicle (n = 10). Throughout the course of treatment, the tumor burden is calculated on a regular basis using the formula (π/6)×d2, where d is the mean tumor diameter measured with a caliper. |
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion Ribociclib is orally bioavailable, highly selective inhibitor of CDK4/6 kinases with inhibitory IC50 concentrations in the low nanomolar range. Following oral dosing, ribociclib was rapidly absorbed with median Tmax ranging from 1 to 5 hours. Plasma concentrations increased approximately 2- to 3-fold from Cycle 1 Day 1 to Cycle 1 Day 18/21 due to accumulation, with steady state reached by approximately Day 8 on the basis of trough concentrations after repeated daily dosing. Dose-proportionality analyses demonstrated that exposure to ribociclib increased with dose, with both Cmax and area under the curve (AUC) increasing slightly more than proportional to dose, over the dose range 50–1,200 mg/day Biological Half-Life 32.6 hours |
| Toxicity/Toxicokinetics |
Hepatotoxicity In the large clinical trials, adverse events were common and led to dose reductions in 45% of patients and discontinuation in 7%. In preregistration clinical trials, ALT elevations occurred in 46% of ribociclib vs 36% of control subjects and elevations above 5 times the ULN in 10% vs 1%. In one study, 1% of recipients developed clinically apparent liver injury with jaundice, but all recovered. The liver injury arose after 3 to 5 cycles and presented with asymptomatic elevations in serum ALT followed by symptoms and jaundice. Immunoallergic and autoimmune features were not present, although liver histology sometimes showed autoimmune hepatitis-like features. Recovery was slow (3 to 5 months), but ultimately complete. Restarting ribociclib resulted in more rapid and severe recurrence. Thus, experience with ribociclib is limited, but it appears to be capable of causing significant liver injury. Likelihood score: C (probable cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the clinical use of ribociclib during breastfeeding. Because protein binding of ribociclib is 70%, clinically important amounts of the drug might pass into breastmilk. The manufacturer recommends that breastfeeding be discontinued during ribociclib therapy and for at least 3 weeks after the final dose. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. |
| References |
[1]. Molecular Pathways: Targeting the Cyclin D-CDK4/6 Axis for Cancer Treatment. Clin Cancer Res. 2015 Jul 1;21(13):2905-10. [2]. Dual CDK4/CDK6 Inhibition Induces Cell-Cycle Arrest and Senescence in Neuroblastoma. Clin Cancer Res. 2013 Nov 15;19(22):6173-82. |
| Additional Infomation |
Cancer cells bypass normal controls over mitotic cell-cycle progression to achieve a deregulated state of proliferation. The retinoblastoma tumor suppressor protein (pRb) governs a key cell-cycle checkpoint that normally prevents G1-phase cells from entering S-phase in the absence of appropriate mitogenic signals. Cancer cells frequently overcome pRb-dependent growth suppression via constitutive phosphorylation and inactivation of pRb function by cyclin-dependent kinase (CDK) 4 or CDK6 partnered with D-type cyclins. Three selective CDK4/6 inhibitors, palbociclib (Ibrance; Pfizer), ribociclib (Novartis), and abemaciclib (Lilly), are in various stages of development in a variety of pRb-positive tumor types, including breast cancer, melanoma, liposarcoma, and non-small cell lung cancer. The emerging, positive clinical data obtained to date finally validate the two decades-old hypothesis that the cyclin D-CDK4/6 pathway is a rational target for cancer therapy.[1] Purpose: Neuroblastoma is a pediatric cancer that continues to exact significant morbidity and mortality. Recently, a number of cell-cycle proteins, particularly those within the Cyclin D/CDK4/CDK6/RB network, have been shown to exert oncogenic roles in neuroblastoma, suggesting that their therapeutic exploitation might improve patient outcomes.[2] Experimental procedures: We evaluated the effect of dual CDK4/CDK6 inhibition on neuroblastoma viability using LEE011 (Novartis Oncology), a highly specific CDK4/6 inhibitor.[2] Results: Treatment with LEE011 significantly reduced proliferation in 12 of 17 human neuroblastoma-derived cell lines by inducing cytostasis at nanomolar concentrations (mean IC50 = 307 ± 68 nmol/L in sensitive lines). LEE011 caused cell-cycle arrest and cellular senescence that was attributed to dose-dependent decreases in phosphorylated RB and FOXM1, respectively. In addition, responsiveness of neuroblastoma xenografts to LEE011 translated to the in vivo setting in that there was a direct correlation of in vitro IC50 values with degree of subcutaneous xenograft growth delay. Although our data indicate that neuroblastomas sensitive to LEE011 were more likely to contain genomic amplification of MYCN (P = 0.01), the identification of additional clinically accessible biomarkers is of high importance. [2] Conclusions: Taken together, our data show that LEE011 is active in a large subset of neuroblastoma cell line and xenograft models, and supports the clinical development of this CDK4/6 inhibitor as a therapy for patients with this disease. Clin Cancer Res; 19(22); 6173-82. ©2013 AACR.[2] |
Solubility Data
| Solubility (In Vitro) |
|
|||
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 0.77 mg/mL (1.63 mM) (saturation unknown) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 7.7 mg/mL clear DMSO stock solution to 400 μL PEG300 and mix evenly; then add 50 μL Tween-80 to the above solution and mix evenly; then add 450 μL normal saline to adjust the volume to 1 mL. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 2: ≥ 0.77 mg/mL (1.63 mM) (saturation unknown) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 7.7 mg/mL clear DMSO stock solution to 900 μL of 20% SBE-β-CD physiological saline solution and mix evenly. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Solubility in Formulation 3: 1 mg/mL (2.12 mM) in PBS (add these co-solvents sequentially from left to right, and one by one), clear solution; with ultrasonication (<60°C). (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.1231 mL | 10.6155 mL | 21.2310 mL | |
| 5 mM | 0.4246 mL | 2.1231 mL | 4.2462 mL | |
| 10 mM | 0.2123 mL | 1.0615 mL | 2.1231 mL |