Physicochemical Properties
| Molecular Formula | C19H35N |
| Molecular Weight | 277.49 |
| Exact Mass | 277.277 |
| CAS # | 6621-47-2 |
| Related CAS # | Perhexiline maleate;6724-53-4 |
| PubChem CID | 4746 |
| Appearance | Typically exists as solid at room temperature |
| Boiling Point | 340ºC at 760 mmHg |
| Flash Point | 164.5ºC |
| LogP | 5.624 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 1 |
| Rotatable Bond Count | 4 |
| Heavy Atom Count | 20 |
| Complexity | 245 |
| Defined Atom Stereocenter Count | 0 |
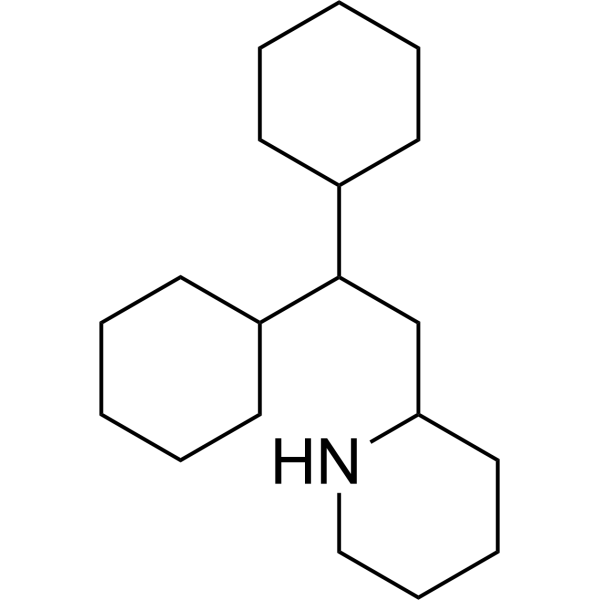
| SMILES | C1CCC(CC1)C(CC2CCCCN2)C3CCCCC3 |
| InChi Key | CYXKNKQEMFBLER-UHFFFAOYSA-N |
| InChi Code | InChI=1S/C19H35N/c1-3-9-16(10-4-1)19(17-11-5-2-6-12-17)15-18-13-7-8-14-20-18/h16-20H,1-15H2 |
| Chemical Name | 2-(2,2-dicyclohexylethyl)piperidine |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| ln Vitro | In HepG2 cells, perhexiline (5–25 μM, 2–6 h) decreases cell viability[2]. In HepG2 cells, perhexiline (5–25 μM, 2–6 h) lowers the amount of cellular ATP and the release of lactate dehydrogenase (LDH)[2]. In HepG2 cells, perhexiline (20 μM, 2 h) activates caspase 3/7[2]. In HepG2 cells, perhexiline (5–25 μM, 4 h) results in mitochondrial dysfunction[2]. Perhexiline (5 μM, 48 h) specifically causes CLL cells (high expression of CPT) to undergo extensive apoptosis[3]. |
| ln Vivo | In female DA rats, perhexiline (200 mg/kg, po, daily for 8 weeks) decreases peripheral neuronal function[4]. In a glioblastoma mouse model, perhexiline (80 mg/kg, oral gavage, for 3 days) exhibits anti-tumor action[5]. |
| Cell Assay |
Cell Viability Assay[2] Cell Types: HepG2 cells Tested Concentrations: 5, 10, 15, 25 μM Incubation Duration: 2, 4, 6 h Experimental Results: Induced time- and concentration-dependent cytotoxicity in hepatic cells. Western Blot Analysis[2] Cell Types: HepG2 cells Tested Concentrations: 5, 10, 15, 25 μM Incubation Duration: 2 h Experimental Results: decreased Bcl-2 and Mcl-1 level, and increased Bad level. |
| Animal Protocol |
Animal/Disease Models: Orthotopic glioblastoma mouse model[5] Doses: 80 mg/kg Route of Administration: po (oral gavage), for 3 days. Experimental Results: Reduces tumor size (MR imaging) and improves in overall survival. |
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion Well absorbed (>80%) from the gastrointestinal tract following oral administration. Metabolism / Metabolites The principal metabolites of perhexiline in man are monohydroxyperhexiline (which is excreted, in part, conjugated with glucuronic acid) and dihydroxyperhexiline that accounts for a relatively small proportion of the total metabolites. Two unidentified metabolites have also been found in the faeces. The pharmacological activity of the metabolites is not known. Hydroxylation of perhexiline is controlled by cytochrome P450 2D6 (CY P450 2D6). The principal metabolites of perhexiline in man are monohydroxyperhexiline (which is excreted, in part, conjugated with glucuronic acid) and dihydroxyperhexiline that accounts for a relatively small proportion of the total metabolites. Two unidentified metabolites have also been found in the faeces. The pharmacological activity of the metabolites is not known. Hydroxylation of perhexiline is controlled by cytochrome P450 2D6 (CY P450 2D6). Half Life: Variable and non-linear. Some reports show a half-life of 2-6 days, others indicate it could be as high as 30 days. Biological Half-Life Variable and non-linear. Some reports show a half-life of 2-6 days, others indicate it could be as high as 30 days. |
| Toxicity/Toxicokinetics |
Toxicity Summary Perhexiline binds to the mitochondrial enzyme carnitine palmitoyltransferase (CPT)-1 and CPT-2. It acts by shifting myocardial substrate utilisation from long chain fatty acids to carbohydrates through inhibition of CPT-1 and, to a lesser extent, CPT-2, resulting in increased glucose and lactate utilization. This results in increased ATP production for the same O2 consumption as before and consequently increases myocardial efficiency. Protein Binding Perhexiline and its metabolites are highly protein bound (>90%). Toxicity Data LD50: 2150 mg/kg (Oral, Rat) (A308) LD50: 2641 mg/kg (Oral, Mouse) (A308) |
| References |
[1]. 27 - Refractory Angina. Chronic Coronary Artery Disease, 2018, 412-431. [2]. Mitochondrial dysfunction and apoptosis underlie the hepatotoxicity of perhexiline. Toxicol In Vitro. 2020 Dec;69:104987. [3]. Elimination of chronic lymphocytic leukemia cells in stromal microenvironment by targeting CPT with an antiangina drug perhexiline. Oncogene. 2016 Oct 27;35(43):5663-5673. [4]. Enantioselectivity in the tissue distribution of perhexiline contributes to different effects on hepatic histology and peripheral neural function in rats. Pharmacol Res Perspect. 2018 Jun;6(3):e00406. [5]. Perhexiline Demonstrates FYN-mediated Antitumor Activity in Glioblastoma. Mol Cancer Ther. 2020 Jul;19(7):1415-1422. |
| Additional Infomation |
Perhexiline is a member of piperidines. It has a role as a cardiovascular drug. Perhexiline is a coronary vasodilator used especially for angina of effort. It may cause neuropathy and hepatitis. Perhexiline is only found in individuals that have used or taken this drug. It is a coronary vasodilator used especially for angina of effort. It may cause neuropathy and hepatitis. [PubChem]Perhexiline binds to the mitochondrial enzyme carnitine palmitoyltransferase (CPT)-1 and CPT-2. It acts by shifting myocardial substrate utilisation from long chain fatty acids to carbohydrates through inhibition of CPT-1 and, to a lesser extent, CPT-2, resulting in increased glucose and lactate utilization. This results in increased ATP production for the same O2 consumption as before and consequently increases myocardial efficiency. 2-(2,2-Dicyclohexylethyl)piperidine. Coronary vasodilator used especially for angina of effort. It may cause neuropathy and hepatitis. Drug Indication For the management of severe angina pectoris. Mechanism of Action Perhexiline binds to the mitochondrial enzyme carnitine palmitoyltransferase (CPT)-1 and CPT-2. It acts by shifting myocardial substrate utilisation from long chain fatty acids to carbohydrates through inhibition of CPT-1 and, to a lesser extent, CPT-2, resulting in increased glucose and lactate utilization. This results in increased ATP production for the same O2 consumption as before and consequently increases myocardial efficiency. Pharmacodynamics Used in the treatment of unresponsive or refractory angina. Perhexiline increases glucose metabolism at the expense of free-fatty-acid metabolism, enhancing oxygen efficiency during myocardial ischaemia. Perhexiline also potentiates platelet responsiveness to nitric oxide both in patients with angina and patients with acute coronary syndrome. The predominant mechanism of this particular perhexiline effect is an increase in platelet cGMP responsiveness. Perhexiline also may reduce the potential for nitric oxide clearance by neutrophil-derived oxygen. Perhexiline relieves symptoms of angina, improves exercise tolerance, and increases the workload needed to induce ischaemia when used as monotherapy. The primary therapeutic roles for perhexiline are as short-term therapy (less than 3 months duration) in patients with severe ischaemia awaiting coronary revascularisation or long-term therapy in patients with ischaemic symptoms refractory to other therapeutic measures. |
Solubility Data
| Solubility (In Vivo) |
Note: Listed below are some common formulations that may be used to formulate products with low water solubility (e.g. < 1 mg/mL), you may test these formulations using a minute amount of products to avoid loss of samples. Injection Formulations (e.g. IP/IV/IM/SC) Injection Formulation 1: DMSO : Tween 80: Saline = 10 : 5 : 85 (i.e. 100 μL DMSO stock solution → 50 μL Tween 80 → 850 μL Saline) *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH ₂ O to obtain a clear solution. Injection Formulation 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL DMSO → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Injection Formulation 3: DMSO : Corn oil = 10 : 90 (i.e. 100 μL DMSO → 900 μL Corn oil) Example: Take the Injection Formulation 3 (DMSO : Corn oil = 10 : 90) as an example, if 1 mL of 2.5 mg/mL working solution is to be prepared, you can take 100 μL 25 mg/mL DMSO stock solution and add to 900 μL corn oil, mix well to obtain a clear or suspension solution (2.5 mg/mL, ready for use in animals). Injection Formulation 4: DMSO : 20% SBE-β-CD in saline = 10 : 90 [i.e. 100 μL DMSO → 900 μL (20% SBE-β-CD in saline)] *Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Injection Formulation 5: 2-Hydroxypropyl-β-cyclodextrin : Saline = 50 : 50 (i.e. 500 μL 2-Hydroxypropyl-β-cyclodextrin → 500 μL Saline) Injection Formulation 6: DMSO : PEG300 : castor oil : Saline = 5 : 10 : 20 : 65 (i.e. 50 μL DMSO → 100 μLPEG300 → 200 μL castor oil → 650 μL Saline) Injection Formulation 7: Ethanol : Cremophor : Saline = 10: 10 : 80 (i.e. 100 μL Ethanol → 100 μL Cremophor → 800 μL Saline) Injection Formulation 8: Dissolve in Cremophor/Ethanol (50 : 50), then diluted by Saline Injection Formulation 9: EtOH : Corn oil = 10 : 90 (i.e. 100 μL EtOH → 900 μL Corn oil) Injection Formulation 10: EtOH : PEG300:Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL EtOH → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Oral Formulations Oral Formulation 1: Suspend in 0.5% CMC Na (carboxymethylcellulose sodium) Oral Formulation 2: Suspend in 0.5% Carboxymethyl cellulose Example: Take the Oral Formulation 1 (Suspend in 0.5% CMC Na) as an example, if 100 mL of 2.5 mg/mL working solution is to be prepared, you can first prepare 0.5% CMC Na solution by measuring 0.5 g CMC Na and dissolve it in 100 mL ddH2O to obtain a clear solution; then add 250 mg of the product to 100 mL 0.5% CMC Na solution, to make the suspension solution (2.5 mg/mL, ready for use in animals). Oral Formulation 3: Dissolved in PEG400 Oral Formulation 4: Suspend in 0.2% Carboxymethyl cellulose Oral Formulation 5: Dissolve in 0.25% Tween 80 and 0.5% Carboxymethyl cellulose Oral Formulation 6: Mixing with food powders Note: Please be aware that the above formulations are for reference only. InvivoChem strongly recommends customers to read literature methods/protocols carefully before determining which formulation you should use for in vivo studies, as different compounds have different solubility properties and have to be formulated differently. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.6037 mL | 18.0187 mL | 36.0373 mL | |
| 5 mM | 0.7207 mL | 3.6037 mL | 7.2075 mL | |
| 10 mM | 0.3604 mL | 1.8019 mL | 3.6037 mL |