Nifurtimox (Bayer-2502; BAY 2502; trade name Lampit) is a 5-nitrofuran based antiprotozoal agent approved for use in the treatment of infections caused by trypanosomes such as Chagas disease and sleeping sickness. It may also be used as a new treatment for neuroblastoma. For sleeping sickness it is used together with eflornithine in nifurtimox-eflornithine combination treatment. In Chagas disease it is a second-line option to benznidazole.
Physicochemical Properties
| Molecular Formula | C10H13N3O5S |
| Molecular Weight | 287.29232 |
| Exact Mass | 287.058 |
| Elemental Analysis | C, 41.81; H, 4.56; N, 14.63; O, 27.85; S, 11.16 |
| CAS # | 23256-30-6 |
| Related CAS # | Nifurtimox-d4 |
| PubChem CID | 6842999 |
| Appearance | Light yellow to yellow solid powder |
| Density | 1.56g/cm3 |
| Boiling Point | 550.3ºC at 760mmHg |
| Melting Point | 177-183 |
| Flash Point | 286.6ºC |
| Vapour Pressure | 3.7E-12mmHg at 25°C |
| Index of Refraction | 1.653 |
| LogP | 2.182 |
| Hydrogen Bond Donor Count | 0 |
| Hydrogen Bond Acceptor Count | 7 |
| Rotatable Bond Count | 2 |
| Heavy Atom Count | 19 |
| Complexity | 467 |
| Defined Atom Stereocenter Count | 0 |
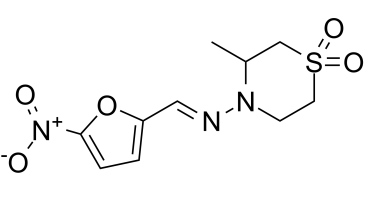
| SMILES | O=S1(CC(C)N(/N=C/C2=CC=C([N+]([O-])=O)O2)CC1)=O |
| InChi Key | ARFHIAQFJWUCFH-IZZDOVSWSA-N |
| InChi Code | InChI=1S/C10H13N3O5S/c1-8-7-19(16,17)5-4-12(8)11-6-9-2-3-10(18-9)13(14)15/h2-3,6,8H,4-5,7H2,1H3/b11-6+ |
| Chemical Name | (E)-3-methyl-4-(((5-nitrofuran-2-yl)methylene)amino)thiomorpholine 1,1-dioxide |
| Synonyms | BAY 2502; Bayer 2502; NIFURTIMOX; Lampit; Bayer 2502; 23256-30-6; Nifurtimoxum; BAY 2502; (+/-)-Nifurtimox; BAYER-2502; Lampit. |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month Note: This product requires protection from light (avoid light exposure) during transportation and storage. In solution, nifurtimox is critically unstable when exposed to light. Therefore, all stock solutions and standard solutions containing nifurtimox should be handled in light-proof containers and reaction tubes. Nifurtimox solutions should be discarded after 7 d. |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | Trypanosoma cruzi; LDH (Lactate dehydrogenase) [1] |
| ln Vitro | Lactate dehydrogenase (LDH) enzyme activity is impacted by furolimus. LDH enzymatic activity was measured 4 hours after 50 µg/mL Nifurtimox administration in order to differentiate between changes in pyruvate metabolism brought on by PDH activation and a decrease in LDH activity. When compared to the untreated control group, the LDH activity of LA-N-1 (P=0.005), IMR-32 (P=0.009), LS (P=0.0035), and SK-N-SH (P=0.0065) was significantly lower. ..In neuroblastoma cells, furtimox decreases cell viability and causes apoptosis and cell cycle arrest. Numerous studies were conducted on four different cell lines to assess the cytotoxic effects of nifurtimox on neuroblastoma. Cell viability for all four neuroblastoma cell lines (LA-N-1, IMR-32 LS, SK-N-, and SH) dropped to an average of 66%, 63%, 62%, and 75% after a 24-hour incubation period at 50 µg/mL. When compared to vehicle controls with DMSO (P<0.05) and untreated controls (P<0.01), this reduction was substantial for all cell lines [1]. |
| ln Vivo | Nifurtimox could competently hinder the development of astroglioma in the mouse brain as compared to temozolomide, the first line of drug for brain tumors. Meanwhile the surviving rate, as well as the body-weight was dramatically upregulated upon nifurtimox treatment, as compared to that of temozolomide. These findings offered nifurtimox as a better alternative drug in treating astroglioma in vivo[2]. |
| Enzyme Assay |
Reactive oxygen species – DCF assay[1] Neuroblastoma cells were treated with nifurtimox as described and were subjected to a flow cytometric analysis of intracellular ROS; 2′,7′-dichlorodihydrofluorescein diacetate (DCF-DA) is taken up into the cells and metabolized to the fluorescent 2′,7′-dichlorofluorescein (DCF) by intracellular ROS. Cells were dyed using the Cellular Reactive Oxygen Species Detection Kit according to the manufacturer's protocol and the intracellular amount of ROS was quantified with a flow cytometer.[1] Western Blot[1] Neuroblastoma cells were treated with nifurtimox as described and indicated. For separation of mitochondrial (determination of (phosphorylated) pyruvate dehydrogenase (PDH, PDH-P)) and cytosolic fraction (determination of N-Myc), 5 × 107 treated cells were homogenized with a dounce tissue grinder. Mitochondria were subsequently extracted using the Mitochondria/Cytosol fractionation kit according to the manufacturer's instructions. |
| Cell Assay |
Cell viability – MTS assay[1] To assess the cell viability after incubation with nifurtimox at different concentrations (10 µg/mL up to 50 µg/mL or 34.8 µM to 174 µM, respectively in the supernatant growth medium) or the vehicle control with according concentrations, all neuroblastoma cell lines were subjected to an MTS assay. Stock solutions of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTS) were made at 480 µM in sterile filtered deionized water and stored at −20°C. Cells were grown to approximately 50% confluency, treated with nifurtimox, and incubated for 1 h with fresh media containing 12 µM MTS. The supernatant was subsequently removed and the cells were lysed with DMSO containing 10% (w/v) sodium dodecyl sulfate (SDS; Carl Roth, #0183) and 1% (v/v) glacial acetic acid. Purple formazan contents of each cell lysate were photometrically analyzed in triplicates at 570 nm (630 nm reference wave length) in 96 microtiter plates. Differentiation of apoptosis and necrosis[1] 50% confluent neuroblastoma cells were treated with nifurtimox as described and dyed with Annexin V (apoptotic cells) and Ethidium homodimer III (necrotic cells) using the Apoptotic/Necrotic Cells Detection Kit according to the manufacturer's instructions. Analysis of cell cycle profiles[1] 50% confluent neuroblastoma cells were treated with nifurtimox as described. Cells were stained using the Nuclear-ID® Green Cell Cycle Kit for flow cytometry according to the manufacturer's protocol. Dyed cells were analyzed in a flow cytometer |
| Animal Protocol |
Establishment and Bioluminescence Detection of Mice Tumor Model for Brain Orthotopic Transplantation [2] Prior to implantation, the U251-luc2-GFP cells were harvested in the logarithmic growth phase, washed with PBS and re-suspended in PBS at the concentration of 2×107 cells/ml. Nude mice were anesthetized and fixed; 20 μl of the cell suspension/per mice (namely 4×105 cells) was injected slightly with a micro-syringe into the right side of the nude mouse brain. The IVIS Spectrum CT imaging system was used to detect bioluminescence at various time points. Briefly, mice were first anesthetized with 2% isoflurane for preparation, and then, transferred into the chamber of IVIS Spectrum CT machine while maintaining the mice with isofluran (0.5%) for sleeping. Bioluminescence images were taken and lastly, the detection signal was quantified with the imaging software coupled with the IVIS Spectrum CT system. 2.7. Design for the Treated Groups and Drug Administration Experiment[2] 7 days after surgical implantation, the tumor-bearing mice were re-imaged with IVIS Spectrum CT machine. A total of 50 mice were randomly divided into 5 groups with 10 mice per group: one normal control group (treated with sodium carboxymethyl cellulose solution), one positive control group (temozolomide 30 mg/kg) and three nifurtimox treated groups at the concentrations of 50 mg/kg, 100 mg/kg and 200 mg/kg. The drugs dissolved in sodium carboxymethyl cellulose solution were administered by gavage for 1 time/day at the dosage of 0.2mL/20g. All animals were daily checked for health conditions and weighed every other day. The bioluminescence signal for the tumor progression was planned for day 1 (7 days after injection), day 6 and day 9 according to the health condition of the individual mice. All treated animals were sacrificed after treatment, brain and tumor block were dissected, weighed and photographed. |
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion The average AUC of nifurtimox is estimated between 1676-2670 μg∙h/L. One pharmacokinetic study of healthy volunteers revealed an AUC of 5430 ng∙ml-1∙h. Cmax ranges between 425-568 μg/L (26–50%) after a single dose of 20 mg with food in adults. Tmax is 4 hours, ranging from 2 to 8 hours post-dose in the fed state. In a pharmacokinetic study of healthy volunteers, serum concentration was low, likely due to the first-pass effect. In the fed state, 44% of the dose was mainly recovered in the urine as metabolites. Fecal and biliary excretion of nifurtimox have not been studied. Nifurtimox crosses the blood-brain barrier and the placenta. One pharmacokinetic study of nifurtimox revealed a clearance of 193.4 l∙h-1. In patients without renal failure; clearance was 99.7 l∙h-1. Metabolism / Metabolites Nifurtimox is largely metabolized via nitroreductase enzymes. Two major inactive metabolites have been identified: M-4 and M-6. The M-4 metabolite is a cysteine conjugate of nifurtimox, while M-6 is likely formed by hydrolytic cleavage of the hydrazone moiety of nifurtimox. Other minor metabolites have also been identified in human plasma. Biological Half-Life The elimination half-life of nifurtimox ranges from 2.4–3.6 hours. A pharmacokinetic study of healthy volunteers and patients with renal failure revealed respective mean half-lives of 2.95 h and 3.95 h. |
| Toxicity/Toxicokinetics |
Hepatotoxicity In multiple prospective controlled trials, nifurtimox therapy was not associated with elevations in aminotransferase or bilirubin levels or with instances of clinically apparent liver injury. Since approval of nifurtimox for American trypanosomiasis, there have been no individual reports of liver injury associated with its use. Likelihood score: E (unlikely cause of clinically apparent liver injury when given in the recommended regimens for Chagas disease). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Limited information indicates that maternal doses of nifurtimox up to 15 mg/kg daily produce do not cause any adverse serious effects in breastfed infants. Breastmilk levels and a computer simulation found that the dose that an exclusively breastfed infant would receive through breastmilk would be much less than the dose given to treat Chagas disease in newborn infants. Other authors consider that breastfeeding is not contraindicated during the use of nifurtimox. ◉ Effects in Breastfed Infants A cohort of 33 infants who were breastfed (extent not stated) by hospitalized mothers taking nifurtimox was followed in the Democratic Republic of the Congo. Thirty mothers took a full course of 30 doses of oral nifurtimox 15 mg/kg daily and all received 14 doses of intravenous eflornithine 400 mg/kg daily for 7 days for human African trypanosomiasis. (sleeping sickness). Nursing mothers also took a median of 4 other concomitant medications, including amoxicillin, ciprofloxacin, metronidazole, trimethoprim-sulfamethoxazole, aspirin, and diclofenac (1 patient each); hydrocortisone, promethazine and quinine (2 patients each); levamisole (6 patients); sulfadoxine-pyrimethamine (8 patients); dipyrone (13 patients); acetaminophen (16 patients); and mebendazole (17 patients). No serious adverse events were reported in any of the breastfed infants. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding The plasma protein binding of nifurtimox is approximately 42%. It is primarily bound to albumin. |
| References |
[1]. Nifurtimox reduces N-Myc expression and aerobic glycolysis in neuroblastoma. Cancer Biol Ther. 2015;16(9):1353-63. |
| Additional Infomation |
Nifurtimox is a nitrofuran antibiotic. Nifurtimox is an antiprotozoal prescription medicine approved by the U.S. Food and Drug Administration (FDA) for the treatment of Chagas disease (American Trypanosomiasis), caused by Trypanosoma cruzi, in children who are less than 18 years of age and weigh at least 5.5 lbs. (2.5 kg). Chagas disease can be an opportunistic infection (OI) of HIV. Chagas disease, caused by a parasite known as Trypanosoma cruzi (T.cruzi), is a vector-transmitted disease affecting animals and humans in the Americas. It is commonly known as American Trypanosomiasis. The CDC estimates that approximately 8 million people in Central America, South America, and Mexico are infected with T. cruzi, without symptoms. If Chagas disease is left untreated, life-threatening sequelae may result. Nifurtimox, developed by Bayer, is a nitrofuran antiprotozoal drug used in the treatment of Chagas disease. On August 6 2020, accelerated FDA approval was granted for its use in pediatric patients in response to promising results from phase III clinical trials. Continued approval will be contingent upon confirmatory data. A convenient feature of Bayer's formulation is the ability to divide the scored tablets manually without the need for pill-cutting devices. Nifurtimox is a nitrofuran antimicrobial agent used to treat Chagas disease (American trypanosomiasis), a chronic protozoal infection due to Trypanosoma cruzi that can lead to severe disability and death from gastrointestinal and cardiac disease. Nifurtimox is rarely associated with serum aminotransferase elevations during therapy and has not been linked to cases of clinically apparent liver injury. Nifurtimox is a nitrofuran derivative with antiprotozoal and potential antineoplastic activities. Nifurtimox is reduced by cytosol enzymes or flavin-containing microsomal enzymes to a highly reactive nitro anion free radical; autooxidation of the nitro anion free radical generates cytotoxic superoxide anion (02-). In addition, nifurtimox-derived nitro anion free radicals may alkylate macromolecules such as nucleic acids and proteins, resulting in the disruption of their structure and function. A nitrofuran thiazine that has been used against TRYPANOSOMIASIS. Drug Indication Nifurtimox is indicated in pediatric patients under 18 weighing at least 2.5 kg. Continued approval of this drug for this indication is dependent upon confirmatory clinical trial results. Treatment of Chagas disease Mechanism of Action The mechanism of action of nifurtimox has not been fully elucidated, however, is believed to occur by the activation of nitroreductase enzymes that produce reactive metabolites with a series of deleterious effects on Trypanosoma cruzi, the parasite causing Chagas disease. The antiprotozoal actions of nifurtimox occur both intracellularly and extracellularly. Inhibition of parasite dehydrogenase activity is another purported mode of action of nifurtimox that warrants further research. Pharmacodynamics Nifurtimox exerts trypanosomal activity against Trypanosoma cruzi, treating Chagas disease. One study reports that nifurtimox and other benzofuran derivatives reduce parasite dehydrogenase activity. Results of a recent phase III clinical trial have shown that a significant number of pediatric patients with acute or chronic Chagas disease treated with nifurtimox were immunoglobulin G (IgG) antibody negative and demonstrated at least a 20% decrease in optical density on two IgG antibody tests for T. cruzi antigens. |
Solubility Data
| Solubility (In Vitro) | DMSO : 57~150 mg/mL (198.4~522.10 mM) |
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 2.5 mg/mL (8.70 mM) (saturation unknown) in 10% DMSO + 40% PEG300 +5% Tween-80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 25.0 mg/mL clear DMSO stock solution to 400 μL PEG300 and mix evenly; then add 50 μL Tween-80 + to the above solution and mix evenly; then add 450 μL normal saline to adjust the volume to 1 mL. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.4808 mL | 17.4040 mL | 34.8080 mL | |
| 5 mM | 0.6962 mL | 3.4808 mL | 6.9616 mL | |
| 10 mM | 0.3481 mL | 1.7404 mL | 3.4808 mL |