Nemorubicin (also known as PNU152243A; Methoxymorpholinyldoxorubicin; PNU 152243; PNU-152243A), an analog of doxorubicin, is a DNA-intercalator, topoisomerase and RNA synthesis inhibitor that was undergoing development for cancer treatment. It was being studied in Phase II clinical trials to treat primary hepatocellular carcinoma. Preclinical evidence demonstrated that nemorubicin has a unique mode of action, overcomes anthracycline resistance, is non-cardiotoxic, and shares structural similarities with doxorubicin. Nemorubicin primarily causes DNA strand breaks via topoisomerase-I cleavage, as we have shown previously. Nemorubicin is ineffective against cells resistant to camptotecins, but it acts as expected against cells resistant to topoisomerase II inhibitors. Furthermore, we discovered that human hepatocytes or microsomes grown in vitro produce a nemorubicin metabolite (PNU-159682) that binds covalently to DNA and is 100 times more cytotoxic than the original compound. In order to gain additional insight into the mechanism of action of nemorubicin, we created an L1210 cell line that is resistant to the drug. We hypothesized that the nucleotide excision repair (NER) system might be involved in mediating the cytotoxic activity of nemorubicin since resistant L1210 cells were more sensitive than the parental cell line to UV irradiation, platinum derivatives, and alkylating agents. We used CHO cell lines that were either proficient or deficient in the excision repair cross-complementing (ERCC) genes, specifically ERCC1 and ERCC6, to test this hypothesis. The NER system may be involved in the induction of nemorubicin cytotoxicity, as evidenced by our finding that nemorubicin is more cytotoxic in NER proficient cells than in deficient ones. Testing PNU-159682 on NER proficient or deficient cells produced comparable results. In conclusion, nemorubicin has a unique mechanism of action that involves the NER system, despite having structural similarities to doxorubicin. This provides justification for clinical combination studies of nemorubicin with alkylating agents or platinum derivatives.
Physicochemical Properties
| Molecular Formula | C32H37NO13 |
| Molecular Weight | 643.63508 |
| Exact Mass | 643.226 |
| Elemental Analysis | C, 59.71; H, 5.79; N, 2.18; O, 32.32 |
| CAS # | 108852-90-0 |
| Related CAS # | Nemorubicin;108852-90-0; 108943-08-4 (HCl) |
| PubChem CID | 65907 |
| Appearance | Red to pink solid powder |
| Density | 1.6±0.1 g/cm3 |
| Boiling Point | 852.2±65.0 °C at 760 mmHg |
| Flash Point | 469.2±34.3 °C |
| Vapour Pressure | 0.0±0.3 mmHg at 25°C |
| Index of Refraction | 1.681 |
| LogP | 4.7 |
| Hydrogen Bond Donor Count | 5 |
| Hydrogen Bond Acceptor Count | 14 |
| Rotatable Bond Count | 7 |
| Heavy Atom Count | 46 |
| Complexity | 1160 |
| Defined Atom Stereocenter Count | 7 |
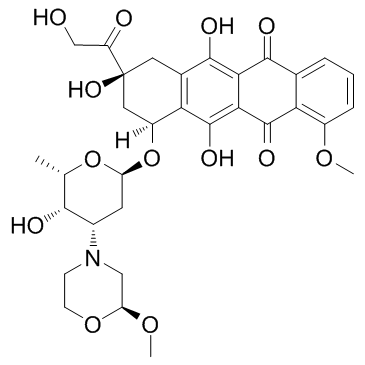
| SMILES | COC1=C2C(C(C3=C(O)C(C[C@](C(CO)=O)(O)C[C@]4([H])O[C@H]5C[C@H](N6CCO[C@H](OC)C6)[C@H](O)[C@H](C)O5)=C4C(O)=C3C2=O)=O)=CC=C1 |
| InChi Key | CTMCWCONSULRHO-UHQPFXKFSA-N |
| InChi Code | InChI=1S/C32H37NO13/c1-14-27(36)17(33-7-8-44-22(12-33)43-3)9-21(45-14)46-19-11-32(41,20(35)13-34)10-16-24(19)31(40)26-25(29(16)38)28(37)15-5-4-6-18(42-2)23(15)30(26)39/h4-6,14,17,19,21-22,27,34,36,38,40-41H,7-13H2,1-3H3/t14-,17-,19-,21-,22-,27+,32-/m0/s1 |
| Chemical Name | (7S,9S)-6,9,11-trihydroxy-9-(2-hydroxyacetyl)-7-[(2R,4S,5S,6S)-5-hydroxy-4-[(2S)-2-methoxymorpholin-4-yl]-6-methyloxan-2-yl]oxy-4-methoxy-8,10-dihydro-7H-tetracene-5,12-dione |
| Synonyms | Methoxymorpholinyldoxorubicin; PNU 152243; PNU-152243A; PNU152243A; PNU-152243A; PNU 152243A; Nemorubicin; Nemorubicin; 108852-90-0; Nemorubicin [INN]; Methoxymorpholino-doxorubicin; Methoxymorpholinyl doxorubicin; FCE-23762; Nemorubicin (GMP); 3'-DESAMINO-3'-(2-METHOXY-4-MORPHOLINYL)-DOXORUBICIN; methoxymorpholinyl-doxorubicin; 3′-deamino-3′-[2″(S)-methoxy-4″-morpholinyl]doxorubicin; MMDX |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | DNA intercalator |
| ln Vitro |
Nemorubicin exhibits antitumor activity against the HT-29, A2780, DU145, EM-2, Jurkat, and CEM cell lines, with IC70s of 578 nM, 468 nM, 193 nM, 191 nM, 68 nM, and 131 ± 9 nM, respectively[1]. Nemorubicin, an anticancer prodrug activated by CYP3A, has the ability to generate PNU-159682, a more potent metabolite[1][2]. Nemorubicin exerts its effects by means of the nucleotide excision repair (NER) system. Compared to L1210/0 cells lacking XPG, NER-preserved L1210/DDP cells exhibit higher levels of nemorubicin (0-0.3 μM) activity. UV damage is more sensitive in cells that are resistant to nemorubicin[3]. Nemorubicin has an IC50 of 0.2 nM, which is 120 times lower than that of 9L cells lacking P450 (IC50, 23.9 nM), indicating that it is cytotoxic to 9L/3A/4 cells. Also, with an IC50 of 1.4 nM, nemoribucicin significantly suppresses Adeno-3A4-infected U251 cells. Nemorubicin is more cytotoxic when P450 reductase is overexpressed[4]. |
| ln Vivo | Nemorubicin is changed into PNU-159682 in rat, mouse, and dog liver microsomes by human liver cytochrome P450 (CYP) 3A4[2]. When administered intravenously (IV) or intratumorally (i.t.) to mice with 9L/3A4 tumors, nemorubicin (60 µg/kg) significantly retards the growth of the tumors, but it has no discernible effect on the tumor growth delay of 9L tumors in scid mice. In mice with 9L/3A4 tumors, nemorubicin (40 µg/kg, i.p.) shows no antitumor activity and no host toxicity[4]. |
| Enzyme Assay |
Nemorubicin (3'-deamino-3'-[2''(S)-methoxy-4''-morpholinyl]doxorubicin; MMDX) is an investigational drug currently in phase II/III clinical testing in hepatocellular carcinoma. A bioactivation product of MMDX, 3'-deamino-3'',4'-anhydro-[2''(S)-methoxy-3''(R)-oxy-4''-morpholinyl]doxorubicin (PNU-159682), has been recently identified in an incubate of the drug with NADPH-supplemented rat liver microsomes. The aims of this study were to obtain information about MMDX biotransformation to PNU-159682 in humans, and to explore the antitumor activity of PNU-159682 . Experimental design: Human liver microsomes (HLM) and microsomes from genetically engineered cell lines expressing individual human cytochrome P450s (CYP) were used to study MMDX biotransformation. We also examined the cytotoxicity and antitumor activity of PNU-159682 using a panel of in vitro-cultured human tumor cell lines and tumor-bearing mice, respectively. Results: HLMs converted MMDX to a major metabolite, whose retention time in liquid chromatography and ion fragmentation in tandem mass spectrometry were identical to those of synthetic PNU-159682. In a bank of HLMs from 10 donors, rates of PNU-159682 formation correlated significantly with three distinct CYP3A-mediated activities. Troleandomycin and ketoconazole, both inhibitors of CYP3A, markedly reduced PNU-159682 formation by HLMs; the reaction was also concentration-dependently inhibited by a monoclonal antibody to CYP3A4/5. Of the 10 cDNA-expressed CYPs examined, only CYP3A4 formed PNU-159682. In addition, PNU-159682 was remarkably more cytotoxic than MMDX and doxorubicin in vitro, and was effective in the two in vivo tumor models tested, i.e., disseminated murine L1210 leukemia and MX-1 human mammary carcinoma xenografts. Conclusions: CYP3A4, the major CYP in human liver, converts MMDX to a more cytotoxic metabolite, PNU-159682, which retains antitumor activity in vivo.[1]
Correlation Studies. [1] Nemorubicin /MMDX (20 μmol/L) was incubated with microsomal fractions from 10 individual human livers; the incubation protocol was the same as that described above. The rates of PNU-159682 formation obtained in these experiments were correlated with several known CYP form-selective catalytic activities evaluated in the same microsomal samples (data provided by BD Gentest except those for nifedipine oxidation and erythromycin N-demethylation). Coefficients of determination (r2) and P values were determined by linear regression analysis. Chemical and Immunochemical Inhibition Studies. [1] Formation of PNU-159682 from 20 μmol/L Nemorubicin /MMDX by pooled HLMs was evaluated in the absence (i.e., control) and presence of known CYP form-selective chemical inhibitors. The following inhibitors were examined at concentrations previously identified as being appropriate to cause CYP form-selective inhibition in HLMs: 7,8-benzoflavone (1 μmol/L, CYP1A2-selective), sulfaphenazole (20 μmol/L, CYP2C9-selective), quinidine (5 μmol/L, CYP2D6-selective), diethyldithiocarbamate (25 μmol/L; CYP2A6/E1-selective), troleandomycin (100 μmol/L, CYP3A-selective) and ketoconazole (1 μmol/L, CYP3A-selective). In experiments with reversible inhibitors, i.e., 7,8-benzoflavone, quinidine, sulfaphenazole, and ketoconazole, the inhibitor was coincubated with the substrate; the incubation protocol was the same as described above. In experiments with mechanism-based inhibitors, i.e., diethyldithiocarbamate and troleandomycin, the inhibitor was preincubated with liver microsomes and NADPH (0.5 mmol) at 37°C for 15 minutes before adding the substrate and additional 0.5 mmol NADPH. The reactions were then conducted as described above. Immunochemical inhibition studies were carried out using mouse ascites fluids containing inhibitory MAbs which have been shown to be specific for different human CYP enzymes. Pooled HLMs (0.25 mg microsomal protein/mL; 20 pmol of total CYP) were preincubated with the designated amount of mouse ascites containing anti-CYP MAb (20-140 μg) at 37°C for 5 minutes in 0.3 mol/L Tris (pH 7.4); the reaction was then initiated by the addition of MMDX (final concentration, 20 μmol/L) and NADPH (final concentration, 0.5 mmol/L) in a total volume of 0.2 mL, and conducted as described above. The highest concentration of each MAb used in these trials (i.e., 7 μg ascites protein/pmol of total CYP) was previously shown to be saturating for an appropriate CYP form-specific reaction in HLMs. Control incubations were carried out in the absence of MAb. Incubation of Nemorubicin /MMDX with cDNA-expressed Human Cytochrome P450 Enzymes [1] Incubations of MMDX with microsomes containing cDNA-expressed CYP enzymes were done as described for HLMs, except that the amount of enzyme used was 50 pmol/mL and incubations were terminated after 60 minutes; substrate concentration was 20 μmol/L. All incubations were done in duplicate. Aliquots of the supernatants from each sample were analyzed for PNU-159682 content by HPLC with fluorescence detection. Nemorubicin (3'-deamino-3'-[2''(S)-methoxy-4''-morpholinyl]doxorubicin; MMDX) is an investigational drug currently in phase II/III clinical testing in hepatocellular carcinoma. A bioactivation product of MMDX, 3'-deamino-3'',4'-anhydro-[2''(S)-methoxy-3''(R)-oxy-4''-morpholinyl]doxorubicin (PNU-159682), has been recently identified in an incubate of the drug with NADPH-supplemented rat liver microsomes. The aims of this study were to obtain information about MMDX biotransformation to PNU-159682 in humans, and to explore the antitumor activity of PNU-159682. Experimental design: Human liver microsomes (HLM) and microsomes from genetically engineered cell lines expressing individual human cytochrome P450s (CYP) were used to study MMDX biotransformation. We also examined the cytotoxicity and antitumor activity of PNU-159682 using a panel of in vitro-cultured human tumor cell lines and tumor-bearing mice, respectively. Results: HLMs converted Nemorubicin /MMDX to a major metabolite, whose retention time in liquid chromatography and ion fragmentation in tandem mass spectrometry were identical to those of synthetic PNU-159682. In a bank of HLMs from 10 donors, rates of PNU-159682 formation correlated significantly with three distinct CYP3A-mediated activities. Troleandomycin and ketoconazole, both inhibitors of CYP3A, markedly reduced PNU-159682 formation by HLMs; the reaction was also concentration-dependently inhibited by a monoclonal antibody to CYP3A4/5. Of the 10 cDNA-expressed CYPs examined, only CYP3A4 formed PNU-159682. In addition, PNU-159682 was remarkably more cytotoxic than MMDX and doxorubicin in vitro, and was effective in the two in vivo tumor models tested, i.e., disseminated murine L1210 leukemia and MX-1 human mammary carcinoma xenografts. Conclusions: CYP3A4, the major CYP in human liver, converts MMDX to a more cytotoxic metabolite, PNU-159682, which retains antitumor activity in vivo.[1] Researchers recently demonstrated that Nemorubicin (MMDX), an investigational antitumor drug, is converted to an active metabolite, PNU-159682, by human liver cytochrome P450 (CYP) 3A4. The objectives of this study were: (1) to investigate MMDX metabolism by liver microsomes from laboratory animals (mice, rats, and dogs of both sexes) to ascertain whether PNU-159682 is also produced in these species, and to identify the CYP form(s) responsible for its formation; (2) to compare the animal metabolism of MMDX with that by human liver microsomes (HLMs), in order to determine which animal species is closest to human beings; (3) to explore whether differences in PNU-159682 formation are responsible for previously reported species- and sex-related differences in MMDX host toxicity. The animal metabolism of MMDX proved to be qualitatively similar to that observed with HLMs since, in all tested species, MMDX was mainly converted to PNU-159682 by a single CYP3A form. However, there were marked quantitative inter- and intra-species differences in kinetic parameters. The mouse and the male rat exhibited V(max) and intrinsic metabolic clearance (CL(int)) values closest to those of human beings, suggesting that these species are the most suitable animal models to investigate MMDX biotransformation. A close inverse correlation was found between MMDX CL(int) and previously reported values of MMDX LD(50) for animals of the species, sex and strain tested here, indicating that differences in the in vivo toxicity of MMDX are most probably due to sex- and species-related differences in the extent of PNU-159682 formation.[2] |
| Cell Assay | Three thousand cells per well in triplicate wells of a 96-well plate are plated with 9L and CHO cells 24 hours before treatment with medication. For four days, different concentrations of IFA or nemorubicin are applied to the cells. After staining the cells with crystal violet (A595), the relative cell survival is computed. Prism 4 is used to calculate IC50 values from a semi-logarithmic graph of the data points[4]. |
| Animal Protocol |
Male ICR/Fox Chase SCID mice are used to grow 9L and 9L/3A4 cells as solid tumors. After being cultivated in DMEM medium to 75% confluence, the cells are trypsinized, rinsed in PBS, and adjusted to 2 × 107 cells/mL of DMEM without added fetal serum. Implantation of either 9L or 9L/3A4 tumor cells is done on four-week-old SCID mice (18–20 g) by injecting 4 × 106 cells/0.2 mL of cell suspension, s.c. on each hind flank. Beginning on the seventh day following tumor implantation, tumor sizes (length and width) are measured twice a week using Vernier calipers. Nemorubicin dissolved in PBS is injected intravenously (IV) or directly intratumorally (i.t.) (three injections spaced seven days apart, each at 60 µg Nemorubicin per kg body weight) when the average tumor size reaches 300 to 400 mm3. Using a 30-gauge needle and a syringe pump set to 1 µL/s, intratumoral injections are administered. Three injections are given for each tumor in an i.t. treatment, with a 50 µL injection volume per tumor per 25 g mouse. In other words, 120 µL of 15 µg/mL of Nemorubicin solution is given to a 30 g mouse, with 20 µL given per site × 3 sites per tumor × 2 tumors/mouse. The same volume of PBS is injected intraperitoneally into drug-free controls. Nemorubicin is injected intraperitoneally (i.p.) at 40 or 60 µg/kg body weight in certain experiments. For the duration of the study, body weight and tumor sizes are measured twice a week. The formula for calculating tumor volumes is V = π/6 (L × W)3/2. The formula for calculating percent tumor regression is 100 × (V1-V2)/V1, where V1 represents the tumor volume on the day of medication treatment and V2 represents the tumor volume on the day that the greatest reduction in tumor size is observed after medication treatment. The amount of time needed for tumors to double in volume following drug treatment is known as the tumor doubling time [4].
Disseminated L1210 Leukemia. [1] Eight-week-old inbred female CD2F1 (BALB/c × DBA/2) were used for evaluation of the therapeutic efficacy of PNU-159682 , in comparison with that of Nemorubicin /MMDX. Disseminated neoplasia was induced by i.v. injection of 105 L1210 cells; 1 day later, the animals were randomly assigned to an experimental group (n = 10) and received a single i.v. injection of MMDX, PNU-159682 , or saline (control group). Treatment efficacy was evaluated by comparing the median survival time in the treated and control groups, and expressed as increase in life span as follows: % increase in life span = (100 × median survival time of drug treated mice / median survival time of control mice) − 100. Statistical comparison between the groups was made using the nonparametric Mann-Whitney test. Subcutaneous MX-1 Human Mammary Adenocarcinoma Xenografts. [1] Four- to six-week-old female CD-1 athymic nude mice were used for evaluation of the activity of PNU-159682 against MX-1 human mammary carcinoma xenografts. On day 0, animals (n = 14) were grafted s.c. with MX-1 tumor fragments in the right flank. Eight days later, they were randomly assigned to the drug treatment group or control group (n = 7 mice per group), and treatment was started. PNU-159682 was given i.v. (4 μg/kg) according to a q7dx3 (every 7 days for three doses) schedule; control animals received saline injections. Tumor volume was estimated from measurements done with a caliper using the formula: tumor volume (mm3) = D × d2 / 2; where D and d are the longest and the shortest diameters, respectively. For ethical reasons, control animals were sacrificed on day 21 when the mean tumor volume in the group was ∼2,500 mm3; animals receiving drug treatment were monitored up to day 50, at which point they were sacrificed. |
| ADME/Pharmacokinetics |
Purpose: Nemorubicin (3'-deamino-3'-[2''(S)-methoxy-4''-morpholinyl]doxorubicin; MMDX) is an investigational drug currently in phase II/III clinical testing in hepatocellular carcinoma. A bioactivation product of MMDX, 3'-deamino-3'',4'-anhydro-[2''(S)-methoxy-3''(R)-oxy-4''-morpholinyl]doxorubicin (PNU-159682), has been recently identified in an incubate of the drug with NADPH-supplemented rat liver microsomes. The aims of this study were to obtain information about MMDX biotransformation to PNU-159682 in humans, and to explore the antitumor activity of PNU-159682.
Experimental design: Human liver microsomes (HLM) and microsomes from genetically engineered cell lines expressing individual human cytochrome P450s (CYP) were used to study MMDX biotransformation. We also examined the cytotoxicity and antitumor activity of PNU-159682 using a panel of in vitro-cultured human tumor cell lines and tumor-bearing mice, respectively.
Results: HLMs converted MMDX to a major metabolite, whose retention time in liquid chromatography and ion fragmentation in tandem mass spectrometry were identical to those of synthetic PNU-159682. In a bank of HLMs from 10 donors, rates of PNU-159682 formation correlated significantly with three distinct CYP3A-mediated activities. Troleandomycin and ketoconazole, both inhibitors of CYP3A, markedly reduced PNU-159682 formation by HLMs; the reaction was also concentration-dependently inhibited by a monoclonal antibody to CYP3A4/5. Of the 10 cDNA-expressed CYPs examined, only CYP3A4 formed PNU-159682. In addition, PNU-159682 was remarkably more cytotoxic than MMDX and doxorubicin in vitro, and was effective in the two in vivo tumor models tested, i.e., disseminated murine L1210 leukemia and MX-1 human mammary carcinoma xenografts.
Conclusions: CYP3A4, the major CYP in human liver, converts MMDX to a more cytotoxic metabolite, PNU-159682, which retains antitumor activity in vivo. [5] We recently demonstrated that nemorubicin (MMDX), an investigational antitumor drug, is converted to an active metabolite, PNU-159682, by human liver cytochrome P450 (CYP) 3A4. The objectives of this study were: (1) to investigate MMDX metabolism by liver microsomes from laboratory animals (mice, rats, and dogs of both sexes) to ascertain whether PNU-159682 is also produced in these species, and to identify the CYP form(s) responsible for its formation; (2) to compare the animal metabolism of MMDX with that by human liver microsomes (HLMs), in order to determine which animal species is closest to human beings; (3) to explore whether differences in PNU-159682 formation are responsible for previously reported species- and sex-related differences in MMDX host toxicity. The animal metabolism of MMDX proved to be qualitatively similar to that observed with HLMs since, in all tested species, MMDX was mainly converted to PNU-159682 by a single CYP3A form. However, there were marked quantitative inter- and intra-species differences in kinetic parameters. The mouse and the male rat exhibited V(max) and intrinsic metabolic clearance (CL(int)) values closest to those of human beings, suggesting that these species are the most suitable animal models to investigate MMDX biotransformation. A close inverse correlation was found between MMDX CL(int) and previously reported values of MMDX LD(50) for animals of the species, sex and strain tested here, indicating that differences in the in vivo toxicity of MMDX are most probably due to sex- and species-related differences in the extent of PNU-159682 formation. [6] |
| References |
[1]. Formation and antitumor activity of PNU-159682, a major metabolite of nemorubicin in human liver microsomes. Clin Cancer Res. 2005 Feb 15;11(4):1608-17. [2]. In vitro hepatic conversion of the anticancer agent nemorubicin to its active metabolite PNU-159682 in mice, rats and dogs: a comparison with human liver microsomes. Biochem Pharmacol. 2008 Sep 15;76(6):784-95. [3]. Down-regulation of the nucleotide excision repair gene XPG as a new mechanism of drug resistance in human and murine cancer cells. Mol Cancer. 2010 Sep 24;9:259. [4]. Potentiation of methoxymorpholinyl doxorubicin antitumor activity by P450 3A4 gene transfer. Cancer Gene Ther. 2009 May;16(5):393-404. [5]. Formation and antitumor activity of PNU-159682, a major metabolite of nemorubicin in human liver microsomes. Clin Cancer Res. 2005 Feb 15;11(4):1608-17. [6]. In vitro hepatic conversion of the anticancer agent nemorubicin to its active metabolite PNU-159682 in mice, rats and dogs: a comparison with human liver microsomes. Biochem Pharmacol. 2008 Sep 15;76(6):784-95. [7]. Down-regulation of the nucleotide excision repair gene XPG as a new mechanism of drug resistance in human and murine cancer cells. Mol Cancer. 2010 Sep 24;9:259. [8]. Lu H, et al. Potentiation of methoxymorpholinyl doxorubicin antitumor activity by P450 3A4 gene transfer. Cancer Gene Ther. 2009 May;16(5):393-404. |
| Additional Infomation |
Nemorubicin is a member of morpholines, an anthracycline antibiotic, a primary alpha-hydroxy ketone and a tertiary alpha-hydroxy ketone. It is functionally related to a doxorubicin. Nemorubicin is a morpholinyl analogue of the anthracycline doxorubicin with antineoplastic activity. Nemorubicin is metabolized via the P450 CYP3A enzyme to a highly cytotoxic derivative. Unlike most anthracyclines, nemorubicin is a topoisomerase I inhibitor and appears to exert its effect through the nucleotide excision repair (NER) system. In addition, this agent does not show cross-resistance with other anthracyclines. We recently demonstrated that nemorubicin (MMDX), an investigational antitumor drug, is converted to an active metabolite, PNU-159682, by human liver cytochrome P450 (CYP) 3A4. The objectives of this study were: (1) to investigate MMDX metabolism by liver microsomes from laboratory animals (mice, rats, and dogs of both sexes) to ascertain whether PNU-159682 is also produced in these species, and to identify the CYP form(s) responsible for its formation; (2) to compare the animal metabolism of MMDX with that by human liver microsomes (HLMs), in order to determine which animal species is closest to human beings; (3) to explore whether differences in PNU-159682 formation are responsible for previously reported species- and sex-related differences in MMDX host toxicity. The animal metabolism of MMDX proved to be qualitatively similar to that observed with HLMs since, in all tested species, MMDX was mainly converted to PNU-159682 by a single CYP3A form. However, there were marked quantitative inter- and intra-species differences in kinetic parameters. The mouse and the male rat exhibited V(max) and intrinsic metabolic clearance (CL(int)) values closest to those of human beings, suggesting that these species are the most suitable animal models to investigate MMDX biotransformation. A close inverse correlation was found between MMDX CL(int) and previously reported values of MMDX LD(50) for animals of the species, sex and strain tested here, indicating that differences in the in vivo toxicity of MMDX are most probably due to sex- and species-related differences in the extent of PNU-159682 formation. Source: Biochem Pharmacol. 2008 Sep 15;76(6):784-95. Antibody drug conjugates (ADCs) normally compose of a humanized antibody and small molecular drug via a chemical linker. After decades of preclinical and clinical studies, a series of ADCs have been widely used for treating specific tumor types in the clinic such as brentuximab vedotin (Adcetris®) for relapsed Hodgkin's lymphoma and systemic anaplastic large cell lymphoma, gemtuzumab ozogamicin (Mylotarg®) for acute myeloid leukemia, ado-trastuzumab emtansine (Kadcyla®) for HER2-positive metastatic breast cancer, inotuzumab ozogamicin (Besponsa®) and most recently polatuzumab vedotin-piiq (Polivy®) for B cell malignancies. More than eighty ADCs have been investigated in different clinical stages from approximately six hundred clinical trials to date. This review summarizes the key elements of ADCs and highlights recent advances of ADCs, as well as important lessons learned from clinical data, and future directions.[3] Background: Targeted EDV nanocells loaded with doxorubicin and microRNA16a have shown excellent safety profiles in Phase I trials in recurrent glioma and mesothelioma. This planned safety analysis of an ongoing first-in-human, open label Phase I/IIa study in patients with treatment-refractory metastatic pancreatic cancer, assesses safety, biologic and clinical activity of EGFR-targeted EDV nanocells carrying cytotoxic drug PNU-159682, designed to overcome drug resistance, combined with EDV nanocells carrying immunomodulatory adjuvant α-galactosyl ceramide, designed to stimulate anti-tumour immune response. Methods: 9 patients with advanced pancreatic cancer enrolled in the dose escalation phase to evaluate safety of the EDV combination. Doses gradually escalated from 2 x 109 EDVs/dose to a maximum of 7 x 109 EDVs/dose in Week 7, with subsequent dosing at the maximum dose achieved in Cycle 1. iRECIST criteria was used to assess tumour response after each cycle, and blood was collected each cycle for cytokine and PBMC analysis. Results: Combination EDVs were well tolerated with no DLTs, and no drug related SAEs. A minority of patients experienced G1 infusion reactions, which responded promptly to supportive treatment. PR or SD was achieved at 8 weeks in 8/9 patients (CBR 89%), with responses confirmed at 4 months in 4/5 evaluable patients (80%), with 2 durable responses seen beyond 6 months. Exploratory analyses have revealed elevation of IFN-α and IFN-γ in almost all evaluable patients (6/8). In addition, we observed elevated CD8+ T cells (2/8), iNKT, dendritic and NK cells (3/8), and a reduction in exhausted CD8+ T cells (3/8), suggesting activation of both innate and adaptive immune responses. Conclusions: EDVs carrying the cytotoxic drug and immune adjuvant are safe and well tolerated. Early signals point to durable responses, possibly related to the development of an innate and adaptive immune response along with cytotoxic effects on drug resistant tumour cells. The Phase IIa study plans to enrol an additional 35 patients to further evaluate safety and anti-tumour efficacy. Clinical trial information: ACTRN12619000385145.[4] |
Solubility Data
| Solubility (In Vitro) | DMSO: ~65 mg/mL (~101 mM) |
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 3.25 mg/mL (5.05 mM) (saturation unknown) in 10% DMSO + 40% PEG300 +5% Tween-80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 32.5 mg/mL clear DMSO stock solution to 400 μL of PEG300 and mix evenly; then add 50 μL of Tween-80 + to the above solution and mix evenly; then add 450 μL of normal saline to adjust the volume to 1 mL. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.5537 mL | 7.7683 mL | 15.5366 mL | |
| 5 mM | 0.3107 mL | 1.5537 mL | 3.1073 mL | |
| 10 mM | 0.1554 mL | 0.7768 mL | 1.5537 mL |