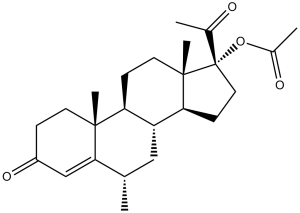
Medroxyprogesterone acetate (formerly NSC26386; NSC 26386; Medroxyprogesterone 17-acetate; MPA), the 17-ester form of Medroxyprogesterone, is a steroidal progestin and a synthetic variant of the human hormone progesterone. It is commonly used as a contraceptive, in hormone replacement therapy and for the treatment of endometriosis. Medroxyprogesterone acetate inhibits the enzyme 3-hydroxyste-roid dehydrogenase, involved in the reversible conversion between 5alpha-dihydroprogesterone and 3alpha, 5alpha-tetrahydroprogesterone.
Physicochemical Properties
| Molecular Formula | C24H34O4 | |
| Molecular Weight | 386.52 | |
| Exact Mass | 386.245 | |
| Elemental Analysis | , 74.58; H, 8.87; O, 16.56 | |
| CAS # | 71-58-9 | |
| Related CAS # | Medroxyprogesterone acetate;71-58-9; 520-85-4 | |
| PubChem CID | 6279 | |
| Appearance | White to off-white solid powder | |
| Density | 1.1±0.1 g/cm3 | |
| Boiling Point | 496.4±45.0 °C at 760 mmHg | |
| Melting Point | 206-207 °C(lit.) | |
| Flash Point | 213.2±28.8 °C | |
| Vapour Pressure | 0.0±1.3 mmHg at 25°C | |
| Index of Refraction | 1.539 | |
| LogP | 4.11 | |
| Hydrogen Bond Donor Count | 0 | |
| Hydrogen Bond Acceptor Count | 4 | |
| Rotatable Bond Count | 3 | |
| Heavy Atom Count | 28 | |
| Complexity | 767 | |
| Defined Atom Stereocenter Count | 7 | |
| SMILES | C[C@H]1C[C@@H]2[C@H](CC[C@]3([C@H]2CC[C@@]3(C(=O)C)OC(=O)C)C)[C@@]4(C1=CC(=O)CC4)C |
|
| InChi Key | PSGAAPLEWMOORI-PEINSRQWSA-N | |
| InChi Code | InChI=1S/C24H34O4/c1-14-12-18-19(22(4)9-6-17(27)13-21(14)22)7-10-23(5)20(18)8-11-24(23,15(2)25)28-16(3)26/h13-14,18-20H,6-12H2,1-5H3/t14-,18+,19-,20-,22+,23-,24-/m0/s1 | |
| Chemical Name | (6S,8R,9S,10R,13S,14S,17R)-17-acetyl-6,10,13-trimethyl-3-oxo-2,3,6,7,8,9,10,11,12,13,14,15,16,17-tetradecahydro-1H-cyclopenta[a]phenanthren-17-yl acetate | |
| Synonyms |
|
|
| HS Tariff Code | 2934.99.9001 | |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | Progesterone receptor; Endogenous Metabolite |
| ln Vitro |
In steroid-deprived HUVEC, medroxyprogesterone acetate (10 and 0.5 nM, 48 hours) suppresses eNOS expression [2]. Medroxyprogesterone acetate (10 and 0.5 nM, 16 hours) decreases the expression of endothelial adhesion molecules (VCAM-1 and ICAM-1 protein), which prevents leukocytes from adhering to human endothelial cells (steroid-deprived HUVEC) [2]. In steroid-deprived HUVEC, medroxyprogesterone acetate (10 and 0.5 nM, 2 hours) decreases NF-κB nuclear translocation [2]. mRNA levels of adhesion molecules in HUVECs treated with medroxyprogesterone acetate (MPA) or 17β-estradiol + MPA were 1.7- to 2.5-fold higher than those in the control. MPA increased the protein expression of E-selectin, P-selectin, and intercellular adhesion molecule-1 compared with that for the control (83.0 ± 0.7, 34.8 ± 1.2, and 5.4 ± 0.0 ng/mL, respectively), whereas other progestogens or 17β-estradiol additive to progestogens did not significantly change expression. MPA significantly increased U937 monocytoid cell adherence compared with the control (56.0 ± 1.5 vs 46.5 ± 3.5 adherent cells per 10 fields) but did not increase adherence to HUVECs with knocked down intercellular adhesion molecule-1. Conclusions: MPA increases cell adhesion molecule expression on HUVECs, causing increased numbers of monocytoid cells to adhere to HUVECs. These MPA effects may be a risk factor for atherogenesis on endothelial cells in postmenopausal women receiving hormone replacement therapy.[2] |
| ln Vivo |
AUC0- 2535.9 ng·h/mL, t1/2 of 10.2 hours, and Cmax of 377.9 ng/mL were observed in rats given 5 mg/kg of medroxyprogesterone acetate by gavage [3]. Over the course of 14 days, rats given oral medroxyprogesterone acetate (0.05-0.2 mg/kg/day) showed an increase in allopregesterone levels in all tissues except the adrenal gland and a change in β-END levels in the hippocampus [4]. Although it can enhance thrombosis, medroxyprogesterone (27.7 μg/day, subcutaneous injection) inhibits arterial vascular thrombosis [3]. MPA and MPA + E2-treated animals showed an aggravated thrombotic response shown by significantly reduced time to stable occlusion. The pro-thrombotic effect of MPA was paralleled by increased ETP whereas platelet activation was not affected. Furthermore, MPA + E2 reduced the number of cells positive for alpha-smooth muscle actin and increased hyaluronan in the plaque matrix. Interestingly, total plaque burden was reduced by MPA but unchanged by MPA + E2.[3]. Conclusion and implications: Long-term treatment with MPA and MPA + E2 increased arterial thrombosis despite inhibitory effects of MPA on atherosclerosis in ApoE-deficient mice. Increased thrombin formation, reduced smooth muscle content and remodelling of non-collagenous plaque matrix may be involved in the pro-thrombotic effects. Thus, MPA exhibits differential effects on arterial thrombosis and on atherosclerosis.[3]. Medroxyprogesterone acetate (MPA) and MPA + E2-treated animals showed an aggravated thrombotic response shown by significantly reduced time to stable occlusion. The pro-thrombotic effect of MPA was paralleled by increased ETP whereas platelet activation was not affected. Furthermore, MPA + E2 reduced the number of cells positive for alpha-smooth muscle actin and increased hyaluronan in the plaque matrix. Interestingly, total plaque burden was reduced by MPA but unchanged by MPA + E2. Conclusion and implications: Long-term treatment with MPA and MPA + E2 increased arterial thrombosis despite inhibitory effects of MPA on atherosclerosis in ApoE-deficient mice. Increased thrombin formation, reduced smooth muscle content and remodelling of non-collagenous plaque matrix may be involved in the pro-thrombotic effects. Thus, MPA exhibits differential effects on arterial thrombosis and on atherosclerosis.[4] |
| Enzyme Assay |
The ovarian hormone progesterone is neuroprotective in different experimental models of neurodegeneration. In the nervous system, progesterone is metabolized to 5alpha-dihydroprogesterone (DHP) by the enzyme 5alpha-reductase. DHP is subsequently reduced to 3alpha,5alpha-tetrahydroprogesterone (THP) by a reversible reaction catalyzed by the enzyme 3alpha-hydroxysteroid dehydrogenase. [5] The mechanism of medroxyprogesterone acetate (MPA)-induced cell proliferation in human breast cancer cells remains elusive. In this study, researchers examined the mechanism by which MPA affects the cyclin D1 expression in progesterone receptor (PR)-positive T47D human breast cancer cells. MPA (10 nM) treatment for 48 h induced proliferation of the cells (1.6-fold induction). MPA induced cyclin D1 expression (3.3-fold induction), and RU486, a selective PR antagonist, blocked the MPA-induced cell proliferation and cyclin D1 expression (23% inhibition). MPA increased both the protein level (2.2-fold induction) and promoter activity (2.7-fold induction) of cyclin D1 in MCF-7 cells transfected with PRB but not with PRA. Although MPA transcriptionally activated cyclin D1 expression, cyclin D1 promoter does not have progesterone-responsive element-related sequence. We further examined the mechanism for the regulation of the cyclin D1 expression. Because the cyclin D1 promoter contains three putative nuclear factor-kappaB (NFkappaB)-binding motifs and NFkappaB is a substrate of Akt, we investigated the effect of the phosphatidylinositol 3-kinase (PI3K)/Akt/NFkappaB cascade on the responses of cyclin D1 to MPA. MPA induced the transient phosphorylation of Akt (2.7-fold induction at 5 min), and treatment with PI3K inhibitor (wortmannin) attenuated the MPA-induced up-regulation of cyclin D1 expression (40% inhibition) and cell proliferation (40% inhibition). MPA also induced phosphorylation of inhibitor of NFkappaBalpha (IkappaBalpha) (2.3-fold induction), and treatment with wortmannin attenuated the MPA-induced IkappaBalpha phosphorylation (60% inhibition). Treatment with an IkappaBalpha phosphorylation inhibitor (BAY 11-7085) or a specific NFkappaB nuclear translocation inhibitor (SN-50) attenuated the MPA-induced up-regulation of both cyclin D1 expression (80 and 50% inhibition, respectively) and cell proliferation (55 and 34% inhibition, respectively). Because MPA induced a transient phosphorylation of Akt and the cyclin D1 promoter contains no progesterone-responsive element-related sequence, the MPA-induced cell proliferation through PRB by up-regulation of cyclin D1 expression via the PI3K/Akt/NFkappaB cascade may be a nongenomic mechanism.[1] The fungal transformations of medroxyrogesterone (1) were investigated for the first time using Cunninghamella elegans, Trichothecium roseum, and Mucor plumbeus. The metabolites obtained are as following: 6β, 20-dihydroxymedroxyprogesterone (2), 12β-hydroxymedroxyprogesterone (3), 6β, 11β-dihydroxymedroxyprogesterone (4), 16β-hydroxymedroxyprogesterone (5), 11α, 17-dihydroxy-6α-methylpregn-4-ene-3, 20-dione (6), 11-oxo-medroxyprogesterone (7), 6α-methyl-17α-hydroxypregn-1,4-diene-3,20-dione (8), and 6β-hydroxymedroxyprogesterone (9), 15β-hydroxymedroxyprogesterone (10), 6α-methyl-17α, 11β-dihydroxy-5α-pregnan-3, 20-dione (11), 11β-hydroxymedroxyprogesterone (12), and 11α, 20-dihydroxymedroxyprogesterone (13). Among all the microbial transformed products, the newly isolated biotransformed product 13 showed the most potent activity against proliferation of SH-SY5Y cells. Compounds 12, 5, 6, 9, 11, and 3 (in descending order of activity) also showed some extent of activity against SH-SY5Y tumour cell line. The never been reported biotransformed product, 2, showed the most potent inhibitory activity against acetylcholinesterase. Molecular modelling studies were carried out to understand the observed experimental activities, and also to obtain more information on the binding mode and the interactions between the biotransformed products, and enzyme.[4] |
| Cell Assay |
Immunofluorescence[2] Cell Types: 100 ng/ml LPS treated endothelial cells Tested Concentrations: 10 and 0.5 nM Incubation Duration: 2h Experimental Results: Inhibited NF-κB nuclear translocation. In HUVECs, adhesion molecule mRNA levels were measured by real-time PCR. Protein expression was quantified by immunocytochemistry and ELISAs. To mimic the monocyte adherence to endothelial cells, we used a flow chamber system to assess progestogen effects on U937 monocytoid cell adherence to HUVEC monolayers. We also examined the suppression effects of adhesion molecules with small interference RNAs.[2] A new thyroid cancer cell line, KTC-2, was established from the malignant pleural effusion of a patient with recurrent thyroid cancer associated with anaplastic transformation from thyroid papillary cancer. Karyotype analysis showed a mode of 109 chromosomes. Subcutaneous cell injections produced small regressing tumors in athymic or severe combined immunodeficiency disorders (SCID) mice. Histologic examination showed anaplastic tumor cells surrounded by prominent mononuclear cells. An expression of thyroglobulin, thyroid transcription factor-1, and PAX-8 but not thyroid peroxidase and thyrotropin (TSH) receptor was detected. Biochemical analysis revealed secretion of interleukin (IL)-6, parathyroid hormone-related protein (PTHrP), and granulocyte-macrophage colony-stimulating factor. All the cytokines are known to induce paraneoplastic syndromes in patients with anaplastic thyroid cancer. Our previous studies revealed that medroxyprogesterone acetate (MPA) reduces secretion of IL-6 and PTHrP from human breast cancer cells. To investigate the regulatory mechanisms of secretion of these cytokines, MPA was administered to the KTC-2 cells. MPA dose-dependently decreased the secretion and mRNA expression of IL-6 and PTHrP. Expression of androgen receptor and glucocorticoid receptor (GR) but not progesterone receptor was detected. Dexamethasone but not dihydrotestosterone and progesterone decreased IL-6 and PTHrP secretion. These findings suggest that MPA decreases IL-6 and PTHrP secretion as a glucocorticoid mediated by GR in the KTC-2 cells. This KTC-2 cell line may be a suitable model for developing new strategies against paraneoplastic syndromes caused by anaplastic thyroid cancer.[6] |
| Animal Protocol |
Apolipoprotein E (ApoE)-/- mice were bilaterally ovariectomized and treated with placebo, MPA (27.7 microg day(-1)) and MPA + 17-beta-oestradiol (E2; 1.1 microg day(-1)) for 90 days, on a Western-type diet. Thrombotic response was measured in a photothrombosis model, platelet activation by fluorescence activated cell sorting (FACS) analysis (CD62P) and thrombin generation by the endogenous thrombin potential (ETP). Furthermore, aortic plaque burden and aortic root plaque composition were determined.[3] Ovariectomy and Hormone Treatment[7] Rats were randomly assigned to one of five treatment groups: Sham (ovary-intact), OVX, OVX+PROG, OVX+Low MPA, and OVX+High MPA. Approximately two months before behavioral testing, all rats received OVX or sham surgery. All rats were anesthetized via isofluorene inhalation. Rats receiving OVX underwent bilateral dorsolateral incisions in the skin and peritoneum, and the ovaries and tips of uterine horns were ligatured and removed. Muscle and skin were then sutured. Rats receiving sham surgery underwent identical skin incision and suture. At the time of surgery, Alzet osmotic pumps (2ML4) containing either proplyene glycol (vehicle), progesterone (PROG; 21 mg dissolved in 2 mL propylene glycol), or MPA (low dose: 14 mg; high dose: 21 mg, dissolved in 2 mL propylene glycol) were implanted in the neck scruff. Hormone administration continued throughout behavior testing and sacrifice. Doses were based on prior research (Zhang, Fishman, and Huang, 1999), multiplied by a factor of 10 to account for the increased weight from the mouse to the rat. After surgery, rats received Rimadyl (5 mg/mL/kg) for pain and saline (2 mL) to prevent dehydration. Animals underwent pump reinsertion surgery every 31–32 days; behavioral testing began 66 days after the first pump insertion. Thus, hormone administration continued throughout behavior testing and sacrifice.[7] |
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion Absorption of oral medroxyprogesterone acetate (MPA) varies considerably between formulations. A 1000mg oral dose reaches an average Cmax of 145-315nmol/L while a 500mg oral dose reaches an average Cmax of 33-178nmol/L with a Tmax of 1-3 hours and a lag time of half an hour. The AUC of a 500mg oral dose of MPA was 543.4-1981.1nmol\*L/h depending on formulation. Intramuscular MPA reaches a Cmax of 4.69±1.52nmol/L with a Tmax of 4.75±2.09 days and an AUC of 81.58±27.64days\*nmol/L. Subcutaneous MPA reaches a Cmax of 3.83±1.56nmol/L with a T±max of 6.52±2.07 days and an AUC of 72.26±38.73days\*nmol/L. However, the pharmacokinetics of MPA may also vary depending on injection site. The majority of medroxyprogesterone acetate (MPA) is eliminated in the urine as glucuronide conjugates and a minority of sulphate conjugates. Glucuronide conjugates are also detected in the feces. Determining the exact ratio of metabolites and parent compound eliminated in the urine and feces is difficult as the metabolite profile in the urine is not significantly different and radio labelling studies are not readily available. The volume of distribution of medroxyprogesterone acetate is 20±3L. The mean clearance of medroxyprogesterone acetate (MPA) is 1668±146L/day or 21.9±4.3L/kg/day. Due to the high inter patient variability in MPA pharmacokinetics, clearance has been reported to be 1600-4000L/day. Metabolism / Metabolites Medroxyprogesterone acetate undergoes beta hydroxylation to form the metabolites 6-beta (M-2), 2-beta (M-4), and 1-beta-hydroxymedroxyprogesterone acetate (M-3). M-2 and M-4 are further metabolized to 2-beta,6-beta-dihydroxymedroxyprogesterone (M-1). M-3 is further metabolized to 1,2-dehydromedroxyprogesterone acetate (M-5). Medroxyprogesterone Acetate has known human metabolites that include M-3, Medroxyprogesterone Acetate, and M-2. Hepatic. Route of Elimination: Following oral dosing, MPA is extensively metabolized in the liver via hydroxylation, with subsequent conjugation and elimination in the urine. Most MPA metabolites are excreted in the urine as glucuronide conjugates with only minor amounts excreted as sulfates. Half Life: 50 days Biological Half-Life Oral medroxyprogesterone acetate (MPA) has an absorption half life of 15-30min and a biological half life of 40-60 hours. Intramuscular MPA has an absorption half life of 0.86±0.30 days and an elimination half life of 24.03±21.74 days. Subcutaneous MPA has an absorption half life of 1.05±0.56 days and an elimination half life of 30.90±15.11 days. |
| Toxicity/Toxicokinetics |
Toxicity Summary Progestins diffuse freely into target cells in the female reproductive tract, mammary gland, hypothalamus, and the pituitary and bind to the progesterone receptor. Once bound to the receptor, progestins slow the frequency of release of gonadotropin releasing hormone (GnRH) from the hypothalamus and blunt the pre-ovulatory LH surge. |
| References |
[1]. Medroxyprogesterone acetate induces cell proliferation through up-regulation of cyclin D1 expression via phosphatidylinositol 3-kinase/Akt/nuclear factor-kappaB cascade in human breast cancer cells. Endocrinology. 2005 Nov;146(11):4917-25. [2]. Medroxyprogesterone acetate enhances monocyte-endothelial interaction under flow conditions by stimulating the expression of cell adhesion molecules. J Clin Endocrinol Metab. 2014 Jun;99(6):2188-97. [3]. Differential effects of medroxyprogesterone acetate on thrombosis and atherosclerosis in mice. Br J Pharmacol. 2009 Dec;158(8):1951-60. [4]. Medroxyprogesterone derivatives from microbial transformation as anti-proliferative agents and acetylcholineterase inhibitors (combined in vitro and in silico approaches). Steroids. 2020 Dec;164:108735. [5]. Reduced metabolites mediate neuroprotective effects of progesterone in the adult rat hippocampus. The synthetic progestin medroxyprogesterone acetate (Provera) is not neuroprotective. J Neurobiol.2006 Aug;66(9):916-28; [6]. Medroxyprogesterone acetate decreases secretion of interleukin-6 and parathyroid hormone-related protein in a new anaplastic thyroid cancer cell line, KTC-2. Thyroid.2003;13(3):249-58; [7]. Medroxyprogesterone acetate impairs memory and alters the GABAergic system in aged surgically menopausal rats. Neurobiol Learn Mem.2010;93(3):444-53. |
| Additional Infomation |
Medroxyprogesterone Acetate can cause cancer according to The World Health Organization's International Agency for Research on Cancer (IARC). It can cause developmental toxicity according to state or federal government labeling requirements. Medroxyprogesterone acetate is an odorless white to off-white microcrystalline powder. (NTP, 1992) Medroxyprogesterone acetate is an acetate ester resulting from the formal condensation of the 17alpha-hydroxy group of medroxyprogesterone with the carboxy group of acetic acid. A widely used progestin in menopausal hormone therapy and in progestogen-only birth control. It has a role as a progestin, an androgen, a female contraceptive drug, a synthetic oral contraceptive, an adjuvant, an inhibitor, an antioxidant and an antineoplastic agent. It is a steroid ester, an acetate ester, a 20-oxo steroid, a 3-oxo-Delta(4) steroid and a corticosteroid. It is functionally related to a medroxyprogesterone. Medroxyprogesterone acetate (MPA) is a [progesterone] derivative that is more resistant to metabolism for improved pharmacokinetic properties. MPA can be use to treat secondary amenorrhea, endometrial hyperplasia, abnormal uterine bleeding, osteoporosis, vasomotor symptoms in menopause, vulvar and vaginal atrophy, prevent pregnancy, manage pain in endometriosis, prevent pregnancy, and is also used in palliative care for endometrial and renal carcinoma. Medroxyprogesterone acetate was granted FDA approval on 18 June 1959. Medroxyprogesterone Acetate is a synthetic, acetate derivative of the sex hormone progesterone. Medroxyprogesterone 17-acetate (NCI04) Medroxyprogesterone acetate (INN, USAN, BAN), also known as 17‘±-hydroxy-6‘±-methylprogesterone acetate, and commonly abbreviated as MPA, is a steroidal progestin, a synthetic variant of the human hormone progesterone. It is used as a contraceptive, in hormone replacement therapy and for the treatment of endometriosis as well as several other indications. MPA is a more potent derivative of its parent compound medroxyprogesterone (MP). While medroxyprogesterone is sometimes used as a synonym for medroxyprogesterone acetate, what is normally being administered is MPA and not MP. A synthetic progestin that is derived from 17-hydroxyprogesterone. It is a long-acting contraceptive that is effective both orally or by intramuscular injection and has also been used to treat breast and endometrial neoplasms. Drug Indication Medroxyprogesterone acetate (MPA) oral tablets are indicated to treat secondary amenorrhea, reduce the incidence of endometrial hyperplasia in postmenopausal women, and to treat abnormal uterine bleeding due to hormonal imbalance, not organic pathology. Oral tablets containing MPA and conjugated estrogens are indicated to prevent postmenopausal osteoporosis and to treat moderate to severe menopausal symptoms such as vasomotor symptoms, vulvar atrophy, and vaginal atrophy. Subcutaneous MPA is indicated to prevent pregnancy and manage pain associated with endometriosis. Intramuscular MPA is indicated to prevent pregnancy, and at higher concentrations for palliative treatment of endometrial or renal carcinoma. FDA Label Mechanism of Action Medroxyprogesterone acetate (MPA) inhibits the production of gonadotropin, preventing follicular maturation and ovulation, which is responsible for it’s ability to prevent pregnancy. This action also thins the endometrium. MPA reduces nuclear estrogen receptors and DNA synthesis in epithelial cells of the endometrium. MPA can also induce p53 dependant apoptosis in certain cancer cell lines, and inhibit GABA-A receptors. Pharmacodynamics Medroxyprogesterone acetate (MPA) inhibits gonadotropin production, reduces nuclear estrogen receptors and DNA synthesis in epithelial cells of the endometrium, and induces p53 dependant apoptosis in cancer cell lines. MPA oral tablets have a half life of 40-60 hours and other formulations can have half lives that are considerably longer, so the duration of action is long. The therapeutic window is wide as patients may take doses ranging from 5mg orally daily to 1000mg as a depo injection weekly. Long term use of MPA is associated with a reduction in bone density and patients who taking MPA during adolescence may have lower peak bone mass than untreated patients, which can also increase the risk of osteoporosis and fractures in the future. |
Solubility Data
| Solubility (In Vitro) |
|
|||
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 1 mg/mL (2.59 mM) (saturation unknown) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 10.0 mg/mL clear DMSO stock solution to 400 μL of PEG300 and mix evenly; then add 50 μL of Tween-80 to the above solution and mix evenly; then add 450 μL of normal saline to adjust the volume to 1 mL. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 2: ≥ 1 mg/mL (2.59 mM) (saturation unknown) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 10.0 mg/mL clear DMSO stock solution to 900 μL of 20% SBE-β-CD physiological saline solution and mix evenly. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Solubility in Formulation 3: ≥ 1 mg/mL (2.59 mM) (saturation unknown) in 10% DMSO + 90% Corn Oil (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 10.0 mg/mL clear DMSO stock solution to 900 μL of corn oil and mix evenly. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5872 mL | 12.9359 mL | 25.8719 mL | |
| 5 mM | 0.5174 mL | 2.5872 mL | 5.1744 mL | |
| 10 mM | 0.2587 mL | 1.2936 mL | 2.5872 mL |