Physicochemical Properties
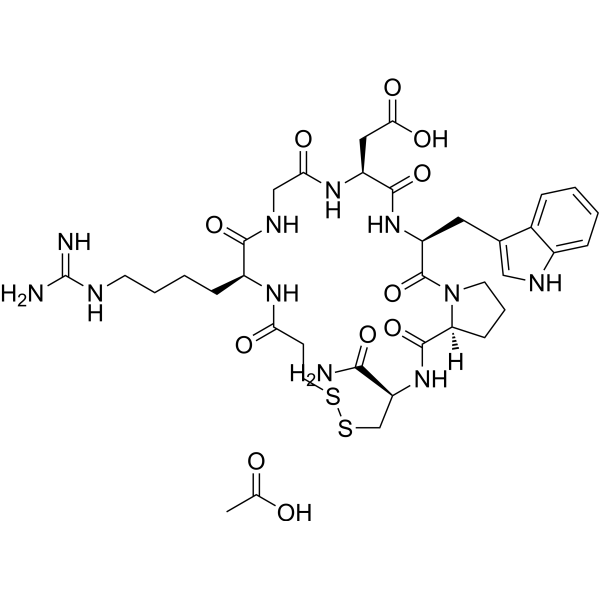
| Molecular Formula | C37H53N11O11S2 |
| Molecular Weight | 831.961864233017 |
| Exact Mass | 891.336 |
| CAS # | 1248559-53-6 |
| Related CAS # | Eptifibatide;188627-80-7 |
| PubChem CID | 12001375 |
| Appearance | Typically exists as solid at room temperature |
| Hydrogen Bond Donor Count | 11 |
| Hydrogen Bond Acceptor Count | 14 |
| Rotatable Bond Count | 10 |
| Heavy Atom Count | 61 |
| Complexity | 1550 |
| Defined Atom Stereocenter Count | 5 |
| SMILES | CC(=O)O.C1C[C@H]2C(=O)N[C@@H](CSSCCC(=O)N[C@H](C(=O)NCC(=O)N[C@H](C(=O)N[C@H](C(=O)N2C1)CC3=CNC4=CC=CC=C43)CC(=O)O)CCCCN=C(N)N)C(=O)N |
| InChi Key | KWKBRYJYRIUYEI-QMYFOHRPSA-N |
| InChi Code | InChI=1S/C35H49N11O9S2.C2H4O2/c36-30(51)25-18-57-56-13-10-27(47)42-22(8-3-4-11-39-35(37)38)31(52)41-17-28(48)43-23(15-29(49)50)32(53)44-24(14-19-16-40-21-7-2-1-6-20(19)21)34(55)46-12-5-9-26(46)33(54)45-25;1-2(3)4/h1-2,6-7,16,22-26,40H,3-5,8-15,17-18H2,(H2,36,51)(H,41,52)(H,42,47)(H,43,48)(H,44,53)(H,45,54)(H,49,50)(H4,37,38,39);1H3,(H,3,4)/t22-,23-,24-,25-,26-;/m0./s1 |
| Chemical Name | acetic acid;2-[(3S,6S,12S,20R,23S)-20-carbamoyl-12-[4-(diaminomethylideneamino)butyl]-3-(1H-indol-3-ylmethyl)-2,5,8,11,14,22-hexaoxo-17,18-dithia-1,4,7,10,13,21-hexazabicyclo[21.3.0]hexacosan-6-yl]acetic acid |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| ln Vitro | Eptifibatide monoacetate is a cyclic heptapeptide that has anti-platelet action and functions as a competitive antagonist for the activated platelet glycoprotein IIb/IIIa receptor[1]. |
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion /MILK/ It is not known whether eptifibatide is distributed into milk in humans. Eptifibatide is approximately 25% bound to plasma proteins, principally (9-16%) to albumin.The volume of distribution of eptifibatide in patients with coronary artery disease is about 185-260 mL/kg and is somewhat higher (220-270 mL/kg) in healthy individuals. Eptifibatide, a synthetic peptide inhibitor of the platelet glycoprotein IIb/IIIa receptor, has been studied as an antithrombotic agent in a variety of acute ischemic coronary syndromes. The purpose of the present study was to characterize the disposition of (14)C-eptifibatide in man after a single intravenous (i.v.) bolus dose. (14)C-Eptifibatide (approximately 50 uCi) was administered to eight healthy men as a single 135-ug/kg IV bolus. Blood, breath carbon dioxide, urine, and fecal samples were collected for up to 72 hours postdose and analyzed for radioactivity by liquid scintillation spectrometry. Plasma and urine samples were also assayed by liquid chromatography with mass spectrometry for eptifibatide and deamidated eptifibatide (DE). Mean (+/- SD) peak plasma eptifibatide concentrations of 879 +/- 251 ng/mL were achieved at the first sampling time (5 minutes), and concentrations then generally declined biexponentially, with a mean distribution half-life of 5 +/- 2.5 minutes and a mean terminal elimination half-life of 1.13 +/- 0.17 hours. Plasma eptifibatide concentrations and radioactivity declined in parallel, with most of the radioactivity (82.4%) attributed to eptifibatide. A total of approximately 73% of administered radioactivity was recovered in the 72-hour period following (14)C-eptifibatide dosing. The primary route of elimination was urinary (98% of the total recovered radioactivity), whereas fecal (1.5%) and breath (0.8%) excretion was small. Eptifibatide is cleared by both renal and nonrenal mechanisms, with renal clearance accounting for approximately 40% of total body clearance. Within the first 24 hours, the drug is primarily excreted in the urine as unmodified eptifibatide (34%), DE (19%), and more polar metabolites (13%). Plasma clearance of eptifibatide is proportional to body weight and estimated creatinine clearance and inversely proportional to age. Following a single IV dose of (14)C-radiolabeled eptifibatide (135 ug/kg) in healthy men, renal clearance averaged approximately 40-50% of total body clearance. Clearance is reduced by 50% in patients with moderate to severe renal impairment (estimated Clcr less than 50 mL/minute). Total body clearance in geriatric patients with coronary artery disease is lower than that in younger adults. For more Absorption, Distribution and Excretion (Complete) data for Eptifibatide (9 total), please visit the HSDB record page. Metabolism / Metabolites (14)C-eptifibatide was extensively metabolized to deamidated eptifibatide and to several polar metabolites by both rats and monkeys. The drug-derived radioactivity excreted into the bile by rats, and identified as deamidated eptifibatide, was reabsorbed from the intestinal tract and further metabolized to more polar metabolites. The plasma and urine metabolite profiles in rats and monkeys indicate that the metabolic disposition of eptifibatide is similar for the two species. Eptifibatide is metabolized principally through deamidation to a metabolite that has approximately 41% of the platelet-aggregation inhibitory activity of the parent compound, and through formation of other more polar metabolites. Approximately 27% of a dose of eptifibatide is broken down in plasma into naturally occurring amino acids; no major non-amino acid metabolites have been detected in plasma in humans. Biological Half-Life In Cynomolgus monkeys, plasma concentrations of (14)C-eptifibatide-derived radioactivity declined with a half life of about 12 hours following a single 2 mg/kg IV dose of (14)C-eptifibatide. Unchanged eptifibatide, which accounted for approximately 93% of total plasma (14)C at 5 min post-dose, was eliminated rapidly with a half life of 17 min. In rats, plasma concentrations of (14)C-eptifibatide-derived radioactivity declined rapidly with a terminal phase half life of about 5 hours following a single 2 mg/kg IV dose of the radiolabeled drug. Unchanged eptifibatide declined with an apparent half life of about 8 min. Following single 2 and 20 mg/kg IV doses, the plasma concentrations of eptifibatide were dose-proportional and the half life (11 to 12 min) was dose-independent, indicating linear kinetics within the 2 to 20 mg/kg dose range. The half-life of eptifibatide in patients with coronary artery disease averages 2.5-2.8 hours. In healthy individuals, half-life of the drug reportedly averages 0.83-2.4 hours. ... The purpose of the present study was to characterize the disposition of (14)C-eptifibatide in man after a single intravenous (IV) bolus dose. (14)C-Eptifibatide (approximately 50 uCi) was administered to eight healthy men as a single 135-ug/kg IV bolus. ... Mean (+/- SD) peak plasma eptifibatide concentrations of 879 +/- 251 ng/mL were achieved at the first sampling time (5 minutes), and concentrations then generally declined biexponentially, with a mean distribution half-life of 5 +/- 2.5 minutes and a mean terminal elimination half-life of 1.13 +/- 0.17 hours. ... |
| Toxicity/Toxicokinetics |
Toxicity Summary IDENTIFICATION AND USE: Eptifibatide, as the drug Integrilin, is indicated to decrease the rate of a combined endpoint of death, new myocardial infarction (MI), or need for urgent intervention in patients undergoing percutaneous coronary intervention (PCI), including those undergoing intracoronary stenting. HUMAN EXPOSURE AND TOXICITY: Limited information is available on the acute toxicity of eptifibatide. In general, overdosage of eptifibatide in humans may be expected to produce effects that are extensions of the pharmacologic effects of the drug, predominantly bleeding. There have been cases of eptifibatide associated thrombocytopenia, which reinforces the importance of platelet count monitoring after therapy with this agent. Eptifibatide was not genotoxic in the human lymphocyte chromosome aberrations test. ANIMAL STUDIES: Single dose toxicity studies were conducted in rats, rabbits and monkeys; doses up to 500 ug/kg/minute administered by continuous intravenous infusion for 90 minutes did not cause mortality and were well-tolerated by all species. In rabbits, a dose-dependent decrease in platelet counts of the 50 and 500 ug/kg/minute (for 90 minutes)-dosed females was attributed to administration of eptifibatide. Findings in the monkeys were limited to petechial hemorrhages in the femoral and/or abdominal regions, which lasted for one to three days. Three out of five monkeys died or were sacrificed during the study due to contusions, excessive bleeding and/or petechial hemorrhages, which resulted in anemia. Total protein albumin and globulin values were reduced in all monkeys. At necropsy, focal hemorrhages in various organs were observed. In a fertility study in rats, dosing with eptifibatide had no effect on the course of pregnancy. No evidence of fertility or parental toxicity nor effects upon parental reproductive performance were observed at daily doses up to 72.0 mg/kg (24 times the maximum recommended daily human dose). Eptifibatide was not genotoxic in the Ames assay at doses up to 667 ug/mL, in the mouse lymphoma cell forward mutation assay at doses up to 1,000 ug/mL, or in the mouse micronucleus test. Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No published information is available on the use of eptifibatide during breastfeeding. Because eptifibatide is a peptide, absorption by the infant is unlikely because it is probably destroyed in the infant's gastrointestinal tract. Until more data become available, eptifibatide should be used with caution during breastfeeding, especially while nursing a newborn or preterm infant. If it is used by a nursing mother, monitor the infant for bruising and bleeding. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Interactions Concomitant use of platelet-aggregation inhibitors and an anticoagulant (particularly in high dosages) may increase the risk of hemorrhage, and careful monitoring for bleeding is necessary, especially at arterial puncture sites. Eptifibatide and concomitant heparin therapy should be discontinued immediately and appropriate therapy (e.g., protamine sulfate in patients receiving heparin) instituted as necessary if serious bleeding occurs (e.g., bleeding not controlled by pressure). In healthy individuals, enoxaparin sodium (1 mg/kg subcutaneously every 12 hours for 4 doses) did not alter the pharmacokinetics or pharmacodynamics (platelet aggregation) of eptifibatide. The manufacturer states that caution should be employed when using eptifibatide with oral anticoagulants. Eptifibatide has been administered concomitantly with thrombolytic agents (e.g., alteplase, streptokinase, tenecteplase) in a limited number of patients with acute myocardial infarction to reduce the risk of reocclusion of the infarct-related artery. Some clinicians suggest that use of short-acting platelet-aggregation inhibitors such as eptifibatide concomitantly with thrombolytic therapy may provide optimal benefit while minimizing the risk of bleeding However, use after thrombolysis of drugs that affect platelet function may increase the risk of bleeding complications, including those requiring blood transfusions, associated with thrombolytic therapy and has not been shown to be unequivocally effective to date; therefore, use of eptifibatide with thrombolytic therapy should be considered investigational and should be undertaken with caution. Limited data from preclinical and clinical studies in patients receiving eptifibatide (0.5 mcg/kg per minute by IV infusion) alone or concomitantly with aspirin, heparin, or both drugs suggest no substantial pharmacokinetic or pharmacodynamic interactions (e.g., additive effects on platelet-aggregation inhibition) between eptifibatide and aspirin. While coadministration of eptifibatide and aspirin resulted in up to a fivefold increase in bleeding time compared with baseline values, similar increases in bleeding time were observed with aspirin and placebo. Nevertheless, since eptifibatide inhibits platelet aggregation, caution should be observed when the drug is used with other drugs that affect hemostasis, including thrombolytic agents, oral anticoagulants, nonsteroidal anti-inflammatory agents (NSAIAs), or dipyridamole. However, clopidogrel or ticlopidine was used routinely with eptifibatide in a large clinical, multicenter study (Enhanced Suppression of the Platelet IIb/IIIa Receptor with Integrilin Therapy (ESPRIT)) in patients undergoing coronary artery stent placement. To minimize potentially additive pharmacologic effects, the manufacturer of eptifibatide states that concomitant therapy with other platelet glycoprotein (GP IIb/IIIa)-receptor inhibitors (e.g., abciximab, tirofiban) should be avoided. |
| References |
[1]. Platelet glycoprotein IIb/IIIa inhibitors in percutaneous coronary intervention: focus on the pharmacokinetic-pharmacodynamic relationships of eptifibatide. Clin Pharmacokinet. 2003;42(8):703-20. |
| Additional Infomation |
Therapeutic Uses Platelet Aggregation Inhibitors /CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Eptifibatide is included in the database. Integrilin is indicated to decrease the rate of a combined endpoint of death or new myocardial infarction (MI) in patients with ACS (unstable angina (UA)/non-ST-elevation myocardial infarction (NSTEMI)), including patients who are to be managed medically and those undergoing percutaneous coronary intervention (PCI). Integrilin is indicated to decrease the rate of a combined endpoint of death, new myocardial infarction (MI), or need for urgent intervention in patients undergoing percutaneous coronary intervention (PCI), including those undergoing intracoronary stenting. /Included in US product label/ Eptifibatide has been administered concomitantly with a thrombolytic agent (e.g., alteplase, tenecteplase) in a limited number of patients to prevent coronary artery reocclusion after an acute myocardial infarction. /NOT included in US product label/ Drug Warnings The most frequent and severe adverse effect of eptifibatide therapy is bleeding. Bleeding complications, which usually are minor and develop at vascular access (e.g., femoral puncture) sites (e.g., in patients undergoing percutaneous coronary intervention (PCI)), have been reported in 35-75% of patients receiving various dosages of eptifibatide in clinical studies. Bleeding is an extension of the pharmacologic action of eptifibatide and was classified in clinical trials principally according to criteria of the Thrombolysis in Myocardial Infarction (TIMI) study groups. Minor bleeding generally was defined as spontaneous gross hematuria or spontaneous hematemesis; observed blood loss with a decrease in hemoglobin concentration of 3-5 g/dL or a reduction in hematocrit of at least 10%; or a decrease of 4-5 g/dL or 12-15% in hemoglobin or hematocrit, respectively, with no identifiable bleeding site. Major bleeding was defined as intracranial hemorrhage or overt bleeding associated with a hemoglobin or hematocrit decrease of at least 5 g/dL or at least 15%, respectively. Because eptifibatide increases the risk of bleeding, the drug is contraindicated in patients with a history of bleeding diathesis or active abnormal bleeding (e.g., elevated hemostatic indices, recent noncompressible vascular punctures GI or genitourinary bleeding) within the previous 30 days. A low hematocrit value (less than 30%) at baseline could represent recent undetected bleeding, and patients with such values may not be able to tolerate additional bleeding episodes; eptifibatide should not be used in these patients. Eptifibatide also is contraindicated in patients with severe uncontrolled hypertension (systolic blood pressure exceeding 200 mm Hg or diastolic blood pressure exceeding 110 mm Hg with antihypertensive therapy); recent (within 6 weeks) major surgery; history of stroke within 30 days or any history of hemorrhagic stroke; current or planned therapy with another GP IIb/IIIa-receptor inhibitor; and patients receiving renal dialysis. No data are available on the use of eptifibatide in patients with serum creatinine concentrations of 4 mg/dL or greater; the dosage should be reduced in patients with serum creatinine concentrations between 2-4 mg/dL. FDA Pregnancy Risk Category: B /NO EVIDENCE OF RISK IN HUMANS. Adequate, well controlled studies in pregnant women have not shown increased risk of fetal abnormalities despite adverse findings in animals, or, in the absence of adequate human studies, animal studies show no fetal risk. The chance of fetal harm is remote but remains a possibility./ Safety and effectiveness of Integrilin in pediatric patients have not been studied. For more Drug Warnings (Complete) data for Eptifibatide (15 total), please visit the HSDB record page. |
Solubility Data
| Solubility (In Vitro) | May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples |
| Solubility (In Vivo) |
Note: Listed below are some common formulations that may be used to formulate products with low water solubility (e.g. < 1 mg/mL), you may test these formulations using a minute amount of products to avoid loss of samples. Injection Formulations (e.g. IP/IV/IM/SC) Injection Formulation 1: DMSO : Tween 80: Saline = 10 : 5 : 85 (i.e. 100 μL DMSO stock solution → 50 μL Tween 80 → 850 μL Saline) *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH ₂ O to obtain a clear solution. Injection Formulation 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL DMSO → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Injection Formulation 3: DMSO : Corn oil = 10 : 90 (i.e. 100 μL DMSO → 900 μL Corn oil) Example: Take the Injection Formulation 3 (DMSO : Corn oil = 10 : 90) as an example, if 1 mL of 2.5 mg/mL working solution is to be prepared, you can take 100 μL 25 mg/mL DMSO stock solution and add to 900 μL corn oil, mix well to obtain a clear or suspension solution (2.5 mg/mL, ready for use in animals). Injection Formulation 4: DMSO : 20% SBE-β-CD in saline = 10 : 90 [i.e. 100 μL DMSO → 900 μL (20% SBE-β-CD in saline)] *Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Injection Formulation 5: 2-Hydroxypropyl-β-cyclodextrin : Saline = 50 : 50 (i.e. 500 μL 2-Hydroxypropyl-β-cyclodextrin → 500 μL Saline) Injection Formulation 6: DMSO : PEG300 : castor oil : Saline = 5 : 10 : 20 : 65 (i.e. 50 μL DMSO → 100 μLPEG300 → 200 μL castor oil → 650 μL Saline) Injection Formulation 7: Ethanol : Cremophor : Saline = 10: 10 : 80 (i.e. 100 μL Ethanol → 100 μL Cremophor → 800 μL Saline) Injection Formulation 8: Dissolve in Cremophor/Ethanol (50 : 50), then diluted by Saline Injection Formulation 9: EtOH : Corn oil = 10 : 90 (i.e. 100 μL EtOH → 900 μL Corn oil) Injection Formulation 10: EtOH : PEG300:Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL EtOH → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Oral Formulations Oral Formulation 1: Suspend in 0.5% CMC Na (carboxymethylcellulose sodium) Oral Formulation 2: Suspend in 0.5% Carboxymethyl cellulose Example: Take the Oral Formulation 1 (Suspend in 0.5% CMC Na) as an example, if 100 mL of 2.5 mg/mL working solution is to be prepared, you can first prepare 0.5% CMC Na solution by measuring 0.5 g CMC Na and dissolve it in 100 mL ddH2O to obtain a clear solution; then add 250 mg of the product to 100 mL 0.5% CMC Na solution, to make the suspension solution (2.5 mg/mL, ready for use in animals). Oral Formulation 3: Dissolved in PEG400 Oral Formulation 4: Suspend in 0.2% Carboxymethyl cellulose Oral Formulation 5: Dissolve in 0.25% Tween 80 and 0.5% Carboxymethyl cellulose Oral Formulation 6: Mixing with food powders Note: Please be aware that the above formulations are for reference only. InvivoChem strongly recommends customers to read literature methods/protocols carefully before determining which formulation you should use for in vivo studies, as different compounds have different solubility properties and have to be formulated differently. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.2020 mL | 6.0099 mL | 12.0198 mL | |
| 5 mM | 0.2404 mL | 1.2020 mL | 2.4040 mL | |
| 10 mM | 0.1202 mL | 0.6010 mL | 1.2020 mL |