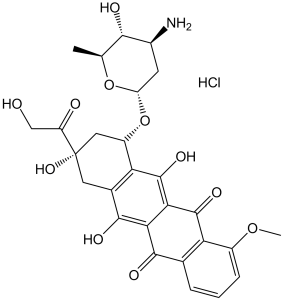
Epirubicin HCl (formerly 4'-epidoxorubicin; epiADR; epidoxorubicin; IMI 28; IMI-28; Ellence; Pharmorubicin PFS), the hydrochloride salt of the 4'-epi-isomer of the anthracycline antineoplastic antibiotic doxorubicin, is a new anthracycline analog and a semisynthetic L-arabino derivative of doxorubicin approved as an anticancer medication. Doxorubicin is a powerful anticancer drug, but its cumulative dose-dependent cardiotoxicity limits its application. Compared to doxorubicin, epirubicin HCl has a better therapeutic index and, at equivalent doses, is less toxic to the heart and blood vessels. Antineoplastic agent epirubicin HCl works by preventing Topoisomerase from doing its job. By intercalating into DNA and interacting with topoisomerase II, epirubicin prevents RNA and protein synthesis as well as DNA replication and repair. In addition, this agent interacts with the lipids in cell membranes to produce toxic free-radical intermediates and lipid peroxidation.
Physicochemical Properties
| Molecular Formula | C27H30CLNO11.HCL |
| Molecular Weight | 579.98 |
| Exact Mass | 579.15 |
| Elemental Analysis | C, 55.91; H, 5.21; Cl, 6.11; N, 2.42; O, 30.34 |
| CAS # | 56390-09-1 |
| Related CAS # | 56390-09-1(HCl salt); 56420-45-2 |
| PubChem CID | 65348 |
| Appearance | Red solid powder |
| Density | 1.61g/cm3 |
| Boiling Point | 810.3ºC at 760 mmHg |
| Melting Point | 185ºC dec |
| Flash Point | 443.8ºC |
| Index of Refraction | 1.709 |
| LogP | 1.503 |
| Hydrogen Bond Donor Count | 7 |
| Hydrogen Bond Acceptor Count | 12 |
| Rotatable Bond Count | 5 |
| Heavy Atom Count | 40 |
| Complexity | 977 |
| Defined Atom Stereocenter Count | 6 |
| SMILES | Cl[H].O([C@@]1([H])C([H])([H])[C@]([H])([C@]([H])(C([H])(C([H])([H])[H])O1)O[H])N([H])[H])[C@]1([H])C2C(=C3C(C4C(=C([H])C([H])=C([H])C=4C(C3=C(C=2C([H])([H])[C@@](C(C([H])([H])O[H])=O)(C1([H])[H])O[H])O[H])=O)OC([H])([H])[H])=O)O[H] |
| InChi Key | MWWSFMDVAYGXBV-FGBSZODSSA-N |
| InChi Code | InChI=1S/C27H29NO11.ClH/c1-10-22(31)13(28)6-17(38-10)39-15-8-27(36,16(30)9-29)7-12-19(15)26(35)21-20(24(12)33)23(32)11-4-3-5-14(37-2)18(11)25(21)34;/h3-5,10,13,15,17,22,29,31,33,35-36H,6-9,28H2,1-2H3;1H/t10-,13-,15-,17-,22-,27-;/m0./s1 |
| Chemical Name | (7S,9S)-7-[(2R,4S,5R,6S)-4-amino-5-hydroxy-6-methyloxan-2-yl]oxy-6,9,11-trihydroxy-9-(2-hydroxyacetyl)-4-methoxy-8,10-dihydro-7H-tetracene-5,12-dione;hydrochloride |
| Synonyms | 4'-epidoxorubicin HCl; 4'-Epidoxorubicin hydrochloride; IMI28; 4-epi DX; EPI; epi DX; 4-epiadriamycin; 4-epidoxorubicin; 4-epidoxorubicin HCl; epiADR; epidoxorubicin; epidorubicin; IMI 28; IMI-28; brand name: Ellence; Pharmorubicin PFS; Pharmorubicin; Farmorubicin; Farmorubicina; Epirubitec; |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month Note: Please store this product in a sealed and protected environment (e.g. under nitrogen), avoid exposure to moisture and light. |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | Topoisomerase | ||
| ln Vitro |
|
||
| ln Vivo |
|
||
| Enzyme Assay |
Reporter assays[2] For the NF-κB-dependent reporter assay, HEK293/NF-κB-RE/Foxp3 cells (1.5×104) or HEK293/NF-κB-RE cells (1.5×104) were seeded into white 96-well plates (Corning) and incubated overnight at 37°C in 5% CO2. These cells were treated with test drugs for 1 h. The cells were then stimulated with 0.3 ng/mL recombinant human TNF-α for 2.5 h. The medium was aspirated off and Steady-Glo (Promega) was added to the cells. The plate was then placed on a shaker for 10 min. Luminescence was detected using an ARVO Light plate reader.[2] Forkhead box protein p3 (Foxp3) is crucial to the development and suppressor function of regulatory T cells (Tregs) that have a significant role in tumor-associated immune suppression. Development of small molecule inhibitors of Foxp3 function is therefore considered a promising strategy to enhance anti-tumor immunity. In this study, we developed a novel cell-based assay system in which the NF-κB luciferase reporter signal is suppressed by the co-expressed Foxp3 protein. Using this system, researchers screened a chemical library consisting of approximately 2,100 compounds and discovered that a cancer chemotherapeutic drug epirubicin restored the Foxp3-inhibited NF-κB activity in a concentration-dependent manner without influencing cell viability. Using immunoprecipitation assay in a Treg-like cell line Karpas-299, we found that epirubicin inhibited the interaction between Foxp3 and p65. In addition, epirubicin inhibited the suppressor function of murine Tregs and thereby improved effector T cell stimulation in vitro. [2] |
||
| Cell Assay |
A 96-well plate is plated with 500 monolayer Hep G2 cells per well. The following day, epirubicin is added to the medium and the cells are treated. 15% volume of MTT dye solution is added at the conclusion of the incubation times. An equal volume of solubilization/stop solution (dimethylsulfoxide) is added to each well for an additional hour of incubation at 37°C after the first hour of incubation. At 570 nm, the reaction solution's absorbance is measured. Epirubicin HCl is a new anthracycline analog and derivative of doxorubicin. Doxorubicin is a potent anticancer agent, the use of which is limited by its cumulative dose-dependent cardiotoxicity. Epirubicin HCl has more favorable therapeutic index than doxorubicin and possesses less hematologic and cardiac toxicity at comparable doses. Hepatoma G2 cells are a valuable model to study hepatocellular carcinoma and the liver, where drugs are metabolized. The goal of our study was to evaluate the cytotoxic effect of epirubicin HCl on viability of Hep G2 cells measured using the MTT cytotoxicity test. Epirubicin HCl produced a concentration- and time-dependent cytotoxicity to Hep G2 cells. The mechanism of cytotoxicity of epirubicin HCl (IC(50) value of 1.6 mug/ml within 24 h) appeared to involve a production of free radical species since activities of free radical scavenging enzymes (SOD, catalase, Se-dependent GPx) were increased. Addition of SOD prevented cytotoxicity of epirubicin HCl, and also counteracted the apoptosis. DNA fragmentation was determined to evaluate apoptosis. Western blot analysis indicated a decrease in GST-pi expression and increased activity of NADPH-dependent cytochrome P450 reductase which is a major enzyme in the conversion of epirubicin HCl to a free radical. It is proposed that production of reactive oxygen species increased by the treatment with epirubicin HCl can cause lipid peroxidation, which subsequently promotes apoptosis and reduces cell viability. Superoxide dismutase, catalase and glutathione peroxidase must be considered as a part of the intracellular antioxidant defense mechanism of Hep G2 cells against single electron reducing quinone-containing anticancer antibiotics.[3] |
||
| Animal Protocol |
|
||
| ADME/Pharmacokinetics |
Absorption
100%
Route of Elimination Epirubicin and its major metabolites are eliminated through biliary excretion and, to a lesser extent, by urinary excretion. Volume of Distribution 21 ± 2 L/kg [60 mg/m2 Dose] 27 ± 11 L/kg [75 mg/m2 Dose] 23 ± 7 L/kg [120 mg/m2 Dose] 21 ± 7 L/kg [150 mg/m2 Dose] Clearance 65 +/- 8 L/hour [Patients1 with Solid Tumors Receiving Intravenous Epirubicin 60 mg/m2] 83 +/- 14 L/hour [Patients1 with Solid Tumors Receiving Intravenous Epirubicin 75 mg/m2] 65 +/- 13 L/hour [Patients1 with Solid Tumors Receiving Intravenous Epirubicin 120 mg/m2] 69 +/- 13 L/hour [Patients1 with Solid Tumors Receiving Intravenous Epirubicin 150 mg/m2] Metabolism / Metabolites Extensively and rapidly metabolized in the liver. Epirubicin is also metabolized by other organs and cells, including red blood cells. The four main metabolic routes are: (1) reduction of the C-13 keto-group with the formation of the 13(S)-dihydro derivative, epirubicinol; (2) conjugation of both the unchanged drug and epirubicinol with glucuronic acid; (3) loss of the amino sugar moiety through a hydrolytic process with the formation of the doxorubicin and doxorubicinol aglycones; and (4) loss of the amino sugar moiety through a redox process with the formation of the 7-deoxy-doxorubicin aglycone and 7-deoxy-doxorubicinol aglycone. Epirubicinol exhibits in vitro cytoxic activity (~10% that of epirubicin), but it is unlikely to reach sufficient concentrations in vivo to produce cytotoxic effects. Epirubicin is extensively and rapidly metabolized by the liver and is also metabolized by other organs and cells, including red blood cells. Four main metabolic routes have been identified: (1) reduction of the C-13 keto-group with the formation of the 13(S)-dihydro derivative, epirubicinol; (2) conjugation of both the unchanged drug and epirubicinol with glucuronic acid; (3) loss of the amino sugar moiety through a hydrolytic process with the formation of the doxorubicin and doxorubicinol aglycones; and (4) loss of the amino sugar moiety through a redox process with the formation of the 7-deoxy-doxorubicin aglycone and 7-deoxy-doxorubicinol aglycone. Epirubicinol has in vitro cytotoxic activity one-tenth that of epirubicin. As plasma levels of epirubicinol are lower than those of the unchanged drug, they are unlikely to reach in vivo concentrations sufficient for cytotoxicity. No significant activity or toxicity has been reported for the other metabolites. NIH; DailyMed. Current Medication Information for Ellence (Epirubicin Hydrochloride) Injection, Solution (Updated: November 2014). Available from, as of June 16, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=0a03c798-a652-4895-b29c-3b521a89ba42 Secondary alcohol metabolites have been proposed to mediate chronic cardiotoxicity induced by doxorubicin (DOX) and other anticancer anthracyclines. In this study, NADPH-supplemented human cardiac cytosol was found to reduce the carbonyl group in the side chain of the tetracyclic ring of doxorubicin, producing the secondary alcohol metabolite doxorubicinol (DOXol). A decrease in the level of alcohol metabolite formation was observed by replacing doxorubicin with epirubicin (EPI), a less cardiotoxic analogue characterized by an axial-to-equatorial epimerization of the hydroxyl group at C-4 in the amino sugar bound to the tetracyclic ring (daunosamine). A similar decrease was observed by replacing doxorubicin with MEN, a novel anthracycline with preclinical evidence of reduced cardiotoxicity. MEN is characterized by the lack of a methoxy group at C-4 in the tetracyclic ring and by intercalation of 2, 6-dideoxy-L-fucose between daunosamine and the aglycone. Multiple comparisons with methoxy- or 4-demethoxyaglycones, and a number of mono- or disaccharide 4-demethoxyanthracyclines, showed that both the lack of the methoxy group and the presence of a disaccharide moiety limited alcohol metabolite formation by MEN. Studies with enzymatically generated or purified anthracycline secondary alcohols also showed that the presence of a disaccharide moiety, but not the lack of a methoxy group, made the metabolite of MEN less reactive with the [4Fe-4S] cluster of cytoplasmic aconitase, as evidenced by its limited reoxidation to the parent carbonyl anthracycline and by a reduced level of delocalization of Fe(II) from the cluster. Collectively, these studies (i) characterize the different influence of methoxy and sugar substituents on the formation and [4Fe-4S] reactivity of anthracycline secondary alcohols, (ii) lend support to the role of alcohol metabolites in anthracycline-induced cardiotoxicity, as they demonstrate that the less cardiotoxic EPI and MEN 10755 share a reduction in the level of formation of such metabolites, and (iii) suggest that the cardiotoxicity of MEN might be further decreased by the reduced [4Fe-4S] reactivity of its alcohol metabolite. Minotti G et al; Chemm Res Toxicol 13 (12): 1336-41 (2000) Many antineoplastic drugs were found to have carcinogenic, mutagenic and teratogenic potential. The aim of this study was to carry out cytogenetic and internal dose monitoring of hospital pharmacy personnel regularly involved in the preparation of cytostatic agents, in order to test possible cytostatics-induced genotoxic effects due to occupational exposure under routine working conditions, and in cases of accidental contamination. ... Platinum in whole blood and anthracyclines in plasma were measured to assess internal exposure to cytostatics. The level of cytogenetic damage was determined in peripheral blood lymphocytes with the micronucleus test and the sister chromatid exchange assay. Five series of monitoring were performed over a period of 2 years. ... No significant differences in the mean frequencies of sister chromatid exchanges (SCE) and micronuclei (MN) were found between occupationally exposed probands and controls (9.9 +/- 1.4 vs 10.1 +/- 1.2 SCEs/cell and 21.2 +/- 7.2 vs 23.3 +/- 7.5 MN/2000 binucleated (BN) cells, n = 16). Significant elevations of SCE or MN were detected in seven out of 12 cases of accidental contamination at the workplace, whereas no increase in platinum in blood and anthracyclines in plasma was observed in these probands. Two cases of non-reported contamination were identified by measurement of epirubicin in plasma. Smoking was found to increase the SCE significantly. No correlation between individual SCE scores and MN scores was observed. ... /The authors/ findings support a transient increase in SCE or MN after relevant exposure to cytostatic drugs in cases of accidental contamination. The lack of significant differences in SCE and MN between hospital pharmacy personnel and unexposed controls, points to high standards of safety at the corresponding workplaces. PMID:11057412 Pilger A et al; Int Arch Occup Environ Health 73 (7): 442-8 (2000) There is compelling in-vitro evidence that the evaluation of doxorubicin or epirubicin pharmacokinetics based solely on plasma concentration may not fully elucidate the differences between the two drugs. Both compounds bind to erythrocytes and their different binding to hemoglobin may influence their disposition in the body. The purpose of the present study was to compare the pharmacokinetics and metabolism of doxorubicin and epirubicin based on the plasma concentration, amount associated with blood cells and simultaneous monitoring of biliary and urinary elimination of unchanged drug and metabolites after single- and multiple-dose injections. The level of sarcoplasmic reticulum Ca2+ATPase in the heart was also measured as a biomarker of cardiotoxicity. Male Sprague-Dawley rats were treated in a parallel design with doxorubicin or epirubicin on a multiple-dosing basis (4 mg kg(-1) per week) or as a single dose injection (20 mg kg(-1)). Blood, urine and bile samples were collected periodically after each dose in the multiple-dosing regimen and the single dose injection, and at the end of each experiment the hearts were removed. The concentrations of each drug in plasma, blood cells, bile and urine samples were determined, and by simultaneous curve-fitting of plasma and bile data according to compartmental analysis, the pharmacokinetic parameters and constants were estimated. The concentration of drug associated with blood cells was analyzed according to non-compartmental analysis. The bile and urine samples provided the in-vivo metabolic data. The level of Ca2+ATPase in the heart, determined by Western blotting, was used as the toxicodynamic parameterto correlate with the kinetic data. Multiple-dosing regimens reduced the total plasma clearance and increased the area under the plasma concentration-time curve of both drugs. Also, the area under the curve of doxorubicin associated with blood cells increased with the weekly doses, and the related mean residence time (MRT) and apparent volume of distribution (Vdss) were steadily reduced. In contrast to doxorubicin, the mean residence time and Vdss of epirubicin increased significantly. Metabolic data indicated significant differences in the level of alcohol and aglycones metabolites. Doxorubicinol and doxorubicin aglycones were significantly greater than epirubicinol and epirubicin aglycone, whereas epirubicinol aglycone was greater than doxorubicinol aglycone. The area under the blood cells concentration-time curve correlated linearly with the changes in Ca2+ATPase net intensity. The results of this study demonstrate the importance of the kinetics of epirubicin and doxorubicin associated with blood cells. Linear correlation between the reduction of net intensity of the biomarker with the area under the curve of doxorubicin associated with blood cells confirms that the differences between the two compounds are related to their interaction with blood cells. This observation together with the observed differences in metabolism may underline a significant role for blood cells in distribution and metabolism of doxorubicin and epirubicin. Ramanathan-Girish S, Boroujerdi M; J Pharmacol 53 (7): 987-97 (2001) Extensively and rapidly metabolized in the liver. Epirubicin is also metabolized by other organs and cells, including red blood cells. The four main metabolic routes are: (1) reduction of the C-13 keto-group with the formation of the 13(S)-dihydro derivative, epirubicinol; (2) conjugation of both the unchanged drug and epirubicinol with glucuronic acid; (3) loss of the amino sugar moiety through a hydrolytic process with the formation of the doxorubicin and doxorubicinol aglycones; and (4) loss of the amino sugar moiety through a redox process with the formation of the 7-deoxy-doxorubicin aglycone and 7-deoxy-doxorubicinol aglycone. Epirubicinol exhibits in vitro cytoxic activity (~10% that of epirubicin), but it is unlikely to reach sufficient concentrations in vivo to produce cytotoxic effects. Route of Elimination: Epirubicin and its major metabolites are eliminated through biliary excretion and, to a lesser extent, by urinary excretion. Half Life: Half-lives for the alpha, beta, and gamma phases of about 3 minutes, 2.5 hours and 33 hours, respectively Biological Half-Life Half-lives for the alpha, beta, and gamma phases of about 3 minutes, 2.5 hours and 33 hours, respectively ... Epirubicin pharmacokinetics may be described by a 3-compartment model, with median half-life values of 3.2 minutes, 1.2 and 32 hours for each phase. ... PMID:8070217 |
||
| Toxicity/Toxicokinetics |
Toxicity Summary
IDENTIFICATION AND USE: Epirubicin is red-orange crystals that are formulated into a solution for intravenous administration. It is used as a component of adjuvant therapy in patients with evidence of axillary node tumor involvement following resection of primary breast cancer. HUMAN EXPOSURE AND TOXICITY: Instances of administration of doses higher than recommended have been reported at doses ranging from 150 to 250 mg/sq m. The observed adverse events in these patients were qualitatively similar to known toxicities of epirubicin. Most of the patients recovered with appropriate supportive care. Secondary acute myelogenous leukemia (AML) has been reported in patients with breast cancer treated with anthracyclines, including epirubicin. Cardiac toxicity, including fatal congestive heart failure (CHF), may occur either during therapy with epirubicin or months to years after termination of therapy. Epirubicin was clastogenic in vitro (chromosome aberrations in human lymphocytes) both in the presence and absence of metabolic activation. ANIMAL STUDIES: Conventional long-term animal studies to evaluate the carcinogenic potential of epirubicin have not been conducted, but intravenous administration of a single 3.6 mg/kg epirubicin dose to female rats approximately doubled the incidence of mammary tumors (primarily fibroadenomas) observed at 1 year. Administration of 0.5 mg/kg epirubicin intravenously to rats every 3 weeks for ten doses increased the incidence of subcutaneous fibromas in males over an 18-month observation period. In addition, subcutaneous administration of 0.75 or 1.0 mg/kg/day to newborn rats for 4 days on both the first and tenth day after birth for a total of eight doses increased the incidence of animals with tumors compared to controls during a 24-month observation period. Administration of 0.8 mg/kg/day intravenously of epirubicin to rats during days 5 to 15 of gestation was embryotoxic (increased resorptions and post-implantation loss) and caused fetal growth retardation (decreased body weight), but was not teratogenic up to this dose. Administration of 2 mg/kg/day intravenously of epirubicin to rats on days 9 and 10 of gestation was embryotoxic (increased late resorptions, post-implantation losses, and dead fetuses; and decreased live fetuses), retarded fetal growth (decreased body weight), and caused decreased placental weight. This dose was also teratogenic, causing numerous external (anal atresia, misshapen tail, abnormal genital tubercle), visceral (primarily gastrointestinal, urinary, and cardiovascular systems), and skeletal (deformed long bones and girdles, rib abnormalities, irregular spinal ossification) malformations. Administration of intravenous epirubicin to rabbits at doses up to 0.2 mg/kg/day during days 6 to 18 of gestation was not embryotoxic or teratogenic, but a maternally toxic dose of 0.32 mg/kg/day increased abortions and delayed ossification. Administration of a maternally toxic intravenous dose of 1 mg/kg/day epirubicin to rabbits on days 10 to 12 of gestation induced abortion, but no other signs of embryofetal toxicity or teratogenicity were observed. When doses up to 0.5 mg/kg/day epirubicin were administered to rat dams from day 17 of gestation to day 21 after delivery, no permanent changes were observed in the development, functional activity, behavior, or reproductive performance of the offspring. In fertility studies in rats, males were given epirubicin daily for 9 weeks and mated with females that were given epirubicin daily for 2 weeks prior to mating and through day 7 of gestation. When dose of 0.3 mg/kg/day was administered to both sexes, no pregnancies resulted. No effects on mating behavior or fertility were observed at 0.1 mg/kg/day, but male rats had atrophy of the testes and epididymis, and reduced spermatogenesis. The 0.1 mg/kg/day dose also caused embryolethality. An increased incidence of fetal growth retardation was observed in these studies at 0.03 mg/kg/day. Multiple daily doses of epirubicin to rabbits and dogs also caused atrophy of male reproductive organs. Single 20.5 and 12 mg/kg doses of intravenous epirubicin caused testicular atrophy in mice and rats, respectively. A single dose of 16.7 mg/kg epirubicin caused uterine atrophy in rats. Epirubicin was mutagenic in vitro to bacteria (Ames test) either in the presence or absence of metabolic activation and to mammalian cells (HGPRT assay in V79 Chinese hamster lung fibroblasts) in the absence but not in the presence of metabolic activation. Epirubicin was clastogenic in vivo (chromosome aberration in mouse bone marrow). Hazardous Substances Data Bank (HSDB) Epirubicin has antimitotic and cytotoxic activity. It inhibits nucleic acid (DNA and RNA) and protein synthesis through a number of proposed mechanisms of action: Epirubicin forms complexes with DNA by intercalation between base pairs, and it inhibits topoisomerase II activity by stabilizing the DNA-topoisomerase II complex, preventing the religation portion of the ligation-religation reaction that topoisomerase II catalyzes. Protein Binding 77% |
||
| References |
[1]. Epirubicin: a review of the pharmacology, clinical activity, and adverse effects of an adriamycin analogue. J Clin Oncol. 1986 Mar;4(3):425-39. [2]. Epirubicin, Identified Using a Novel Luciferase Reporter Assay for Foxp3 Inhibitors, Inhibits Regulatory T Cell Activity. PLoS One. 2016 Jun 10;11(6):e0156643. [3]. Epirubicin HCl toxicity in human-liver derived hepatoma G2 cells. Pol J Pharmacol, 2004. 56(4): p. 435-44. [4]. Drugs ten years later: epirubicin. Ann Oncol, 1993. 4(5): p. 359-69. [5]. Antitumor activity of paclitaxel and epirubicin in human breast carcinoma, R-27. Folia Microbiol (Praha), 1998. 43(5): p. 473-4. |
||
| Additional Infomation |
Epirubicin Hydrochloride is the hydrochloride salt of the 4'-epi-isomer of the anthracycline antineoplastic antibiotic doxorubicin. Epirubicin intercalates into DNA and inhibits topoisomerase II, thereby inhibiting DNA replication and ultimately, interfering with RNA and protein synthesis. This agent also produces toxic free-radical intermediates and interacts with cell membrane lipids causing lipid peroxidation. An anthracycline which is the 4'-epi-isomer of doxorubicin. The compound exerts its antitumor effects by interference with the synthesis and function of DNA. See also: Epirubicin (has active moiety). 4'-epidoxorubicin is an anthracycline that is the 4'-epi-isomer of doxorubicin. It has a role as an EC 5.99.1.3 [DNA topoisomerase (ATP-hydrolysing)] inhibitor, an antineoplastic agent and an antimicrobial agent. It is an anthracycline, a deoxy hexoside, an anthracycline antibiotic, an aminoglycoside, a monosaccharide derivative, a member of p-quinones, a primary alpha-hydroxy ketone and a tertiary alpha-hydroxy ketone. It is functionally related to a doxorubicin. It is a conjugate acid of a 4'-epidoxorubicinium. An anthracycline which is the 4'-epi-isomer of doxorubicin. The compound exerts its antitumor effects by interference with the synthesis and function of DNA. Epirubicin is an Anthracycline Topoisomerase Inhibitor. The mechanism of action of epirubicin is as a Topoisomerase Inhibitor. Epirubicin has been reported in Bos taurus, Lasiodiplodia theobromae, and other organisms with data available. Epirubicin is a 4'-epi-isomer of the anthracycline antineoplastic antibiotic doxorubicin. Epirubicin intercalates into DNA and inhibits topoisomerase II, thereby inhibiting DNA replication and ultimately, interfering with RNA and protein synthesis. This agent also produces toxic free-radical intermediates and interacts with cell membrane lipids causing lipid peroxidation. Epirubicin is only found in individuals that have used or taken this drug. It is an anthracycline which is the 4'-epi-isomer of doxorubicin. The compound exerts its antitumor effects by interference with the synthesis and function of DNA. Epirubicin has antimitotic and cytotoxic activity. It inhibits nucleic acid (DNA and RNA) and protein synthesis through a number of proposed mechanisms of action: Epirubicin forms complexes with DNA by intercalation between base pairs, and it inhibits topoisomerase II activity by stabilizing the DNA-topoisomerase II complex, preventing the religation portion of the ligation-religation reaction that topoisomerase II catalyzes. It also interferes with DNA replication and transcription by inhibiting DNA helicase activity. An anthracycline which is the 4'-epi-isomer of doxorubicin. The compound exerts its antitumor effects by interference with the synthesis and function of DNA. See also: Epirubicin Hydrochloride (has salt form). Drug Indication For use as a component of adjuvant therapy in patients with evidence of axillary node tumor involvement following resection of primary breast cancer. FDA Label Mechanism of Action Epirubicin has antimitotic and cytotoxic activity. It inhibits nucleic acid (DNA and RNA) and protein synthesis through a number of proposed mechanisms of action: Epirubicin forms complexes with DNA by intercalation between base pairs, and it inhibits topoisomerase II activity by stabilizing the DNA-topoisomerase II complex, preventing the religation portion of the ligation-religation reaction that topoisomerase II catalyzes. It also interferes with DNA replication and transcription by inhibiting DNA helicase activity. Epirubicin is an anthracycline cytotoxic agent. Although it is known that anthracyclines can interfere with a number of biochemical and biological functions within eukaryotic cells, the precise mechanisms of epirubicin's cytotoxic and/or antiproliferative properties have not been completely elucidated. Epirubicin forms a complex with DNA by intercalation of its planar rings between nucleotide base pairs, with consequent inhibition of nucleic acid (DNA and RNA) and protein synthesis. Such intercalation triggers DNA cleavage by topoisomerase II, resulting in cytocidal activity. Epirubicin also inhibits DNA helicase activity, preventing the enzymatic separation of double-stranded DNA and interfering with replication and transcription. Epirubicin is also involved in oxidation/reduction reactions by generating cytotoxic free radicals. The antiproliferative and cytotoxic activity of epirubicin is thought to result from these or other possible mechanisms. Epirubicin fights cancer through topoisomerase II inhibition, hence producing DNA strand breaks that finally lead to cell apoptosis. But anthracyclines produce free radicals that may explain their adverse effects. Dexrazoxane--an iron chelator--was proven to decrease free radical production and anthracycline cardiotoxicity. In this article, we report the concentrations of cellular 8-oxo-7,8-dihydro-2'-deoxyguanosine (8-oxo-dGuo) relative to 2'-deoxyguanosine (dGuo), and comet assay results from a study including 20 cancer patients treated with epirubicin. Plasma concentrations of vitamins A, E, C and carotenoids are also reported. All data were obtained before and immediately after epirubicin infusion. The ratios of 8-Oxo-dGuo to dGuo were measured in leukocyte DNA by HPLC-coulometry after NaI extraction of nucleic acids. Vitamins A and E and carotenoids were measured by HPLC-spectrophotometry. Vitamin C was measured by HPLC-spectrofluorimetry. Median 8-oxo-dGuo/dGuo ratios increased significantly from 0.34 to 0.48 lesions per 100,000 bases while per cent of tail DNA increased from 3.47 to 3.94 after chemotherapy 8-Oxo-dGuo/dGuo and per cent of tail DNA medians remained in the normal range. Only vitamin C decreased significantly from 55.4 to 50.3 microM Decreases in vitamins A, E, lutein and zeaxanthin were not significant, but concentrations were below the lower limit of the normal range both before and after chemotherapy. Only the correlation between comet assay results and vitamin C concentrations was significant (rho =-0.517, p = 0.023). This study shows that cellular DNA is damaged by epirubicin-generated free radicals which produce the mutagenic modified base 8-oxo-dGuo and are responsible for strand breaks. However, strand breaks are created not only by free radicals but also by topoisomerase II inhibition. In a previous study we did not find any significant change in urinary 8-oxo-dGuo excretion after adriamycin treatment. However, 8-oxo-dGuo may have increased at the end of urine collection as DNA repair and subsequent kidney elimination are relatively slow processes. In another study, authors used GC-MS to detect 8-oxo-dGuo in DNA and did not find any change after prolonged adriamycin infusion. Reasons for these apparent discrepancies are discussed. |
Solubility Data
| Solubility (In Vitro) |
|
|||
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 2.5 mg/mL (4.31 mM) (saturation unknown) in 5% DMSO + 40% PEG300 + 5% Tween80 + 50% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 2: ≥ 2.5 mg/mL (4.31 mM) (saturation unknown) in 5% DMSO + 95% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Solubility in Formulation 3: ≥ 2.08 mg/mL (3.59 mM) (saturation unknown) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 20.8 mg/mL clear DMSO stock solution to 400 μL PEG300 and mix evenly; then add 50 μL Tween-80 to the above solution and mix evenly; then add 450 μL normal saline to adjust the volume to 1 mL. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 4: ≥ 0.5 mg/mL (0.86 mM) (saturation unknown) in 1% DMSO 99% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 5: 1.1 mg/mL (1.90 mM) in PBS (add these co-solvents sequentially from left to right, and one by one), clear solution; with ultrasonication. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.7242 mL | 8.6210 mL | 17.2420 mL | |
| 5 mM | 0.3448 mL | 1.7242 mL | 3.4484 mL | |
| 10 mM | 0.1724 mL | 0.8621 mL | 1.7242 mL |