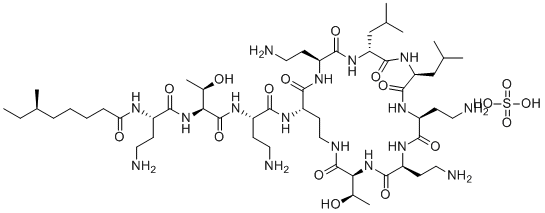
Colistin sulfate (Belcomycin; Polymixin E), originally isolated from B. polymyxa, is a polypeptide antibiotic and apoptosis inducer, also acts as a NADH quinone oxidoreductase inhibitor. It inhibits gram-negative bacteria by binding to lipopolysaccharides and phospholipids in the outer cell membrane of gram-negative bacteria.
Physicochemical Properties
| Molecular Formula | C52H98N16O13.2.5H2O4S |
| Molecular Weight | 1400.64 |
| Exact Mass | 1,266.73 |
| Elemental Analysis | C, 50.22; H, 8.11; N, 17.68; O, 21.46; S, 2.53 |
| CAS # | 1264-72-8 |
| Related CAS # | Colistin;1066-17-7 |
| Appearance | White to off-white solid powder |
| Density | 1.3±0.1 g/cm3 |
| Boiling Point | 1537.3±65.0 °C at 760 mmHg |
| Melting Point | 200-220°C |
| Flash Point | 883.5±34.3 °C |
| Vapour Pressure | 0.0±0.6 mmHg at 25°C |
| Index of Refraction | 1.575 |
| LogP | -3.68 |
| SMILES | CCC(C)CCCC(N[C@@H](CCN)C(N[C@H](C(N[C@H](C(N[C@@H](CCNC([C@H]([C@H](O)C)N1)=O)C(N[C@@H](CCN)C(N[C@H](CC(C)C)C(N[C@@H](CC(C)C)C(N[C@@H](CCN)C(N[C@@H](CCN)C1=O)=O)=O)=O)=O)=O)=O)CCN)=O)[C@H](O)C)=O)=O.O=S(O)(O)=O |
| InChi Key | ZJIWRHLZXQPFAD-FPSDIOKYSA-N |
| Chemical Name | (R)-N-((S)-4-amino-1-(((2S,3R)-1-(((S)-4-amino-1-oxo-1-(((3S,6S,9S,12S,15R,18S,21S)-6,9,18-tris(2-aminoethyl)-3-((R)-1-hydroxyethyl)-12,15-diisobutyl-2,5,8,11,14,17,20-heptaoxo-1,4,7,10,13,16,19-heptaazacyclotricosan-21-yl)amino)butan-2-yl)amino)-3-hydroxy-1-oxobutan-2-yl)amino)-1-oxobutan-2-yl)-6-methyloctanamide sulfate |
| Synonyms | Belcomycin; Polymixin E; Colistin sulfate |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month Note: Please store this product in a sealed and protected environment, avoid exposure to moisture. |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | Bacterial cell wall synthessis; lipopolysaccharides and phospholipids in the outer cell membrane of gram-negative bacteria |
| ln Vitro | Colistins work like detergents to kill gram-negative bacteria. This mechanism includes competitively displacing divalent cations (calcium and magnesium) from the negatively charged phosphate groups of membrane lipids, as well as interaction with the lipopolysaccharides and phospholipids of the outer membrane through electrostatic interference[1]. Colistin, also known as polymyxin E, is a good treatment for infections brought on by gram-negative bacteria that are resistant to many drugs because of its quick bacterial killing, limited spectrum of action, and concomitant delayed development of resistance. Commercially, colistin comes in two forms: colistin methanesulfonate (sodium) for parenteral use and colistin (sulfate), primarily for topical use[2]. |
| ln Vivo |
Following intraperitoneal instillation, slow and sustained CMS conversion leads to high concentrations of colistin in rat ELF[3]. Piglets are frequently given colonistin, however both under- and overdosing are common. The fecal microbiota of piglets is not significantly disrupted by colistin overdoses or underdoses, and chromosomal resistance in the predominant E. coli population is seldom selected for[4]. Colistin methanesulfonate (CMS), the inactive prodrug of colistin, is administered by inhalation for the management of respiratory infections. However, limited pharmacokinetic data are available for CMS and colistin following pulmonary delivery. This study investigates the pharmacokinetics of CMS and colistin following intravenous (i.v.) and intratracheal (i.t.) administration in rats and determines the targeting advantage after direct delivery into the lungs. In addition to plasma, bronchoalveolar lavage (BAL) fluid was collected to quantify drug concentrations in lung epithelial lining fluid (ELF). The resulting data were analyzed using a population modeling approach in S-ADAPT. A three-compartment model described the disposition of both compounds in plasma following i.v. administration. The estimated mean clearance from the central compartment was 0.122 liters/h for CMS and 0.0657 liters/h for colistin. Conversion of CMS to colistin from all three compartments was required to fit the plasma data. The fraction of the i.v. dose converted to colistin in the systemic circulation was 0.0255. Two BAL fluid compartments were required to reflect drug kinetics in the ELF after i.t. dosing. A slow conversion of CMS (mean conversion time [MCTCMS] = 3.48 h) in the lungs contributed to high and sustained concentrations of colistin in ELF. The fraction of the CMS dose converted to colistin in ELF (fm,ELF = 0.226) was higher than the corresponding fractional conversion in plasma after i.v. administration. In conclusion, pulmonary administration of CMS achieves high and sustained exposures of colistin in lungs for targeting respiratory infections[3]. |
| Enzyme Assay |
MIC determination.[2] MICs were determined by both broth macrodilution and microdilution in cation-adjusted Mueller-Hinton broth ccording to NCCLS standards (16). Strains were considered resistant to colistin and colistin methanesulfonate if the MICs were ≥32 mg/liter. Time-kill kinetics.[2] The time-kill kinetics of four strains, ATCC 27853 and three clinical isolates, two of which were mucoid, were examined. The clinical isolates were selected in order to have a range of MICs within the susceptible category. The MICs of colistin and colistin methanesulfonate, respectively, for the four strains were as follows: ATCC 27853, 4 and 16 mg/liter; 18982, 4 and 8 mg/liter; 19056, 1 and 8 mg/liter; and 20223, 4 and 16 mg/liter. Colistin and colistin methanesulfonate were added to a logarithmic-phase broth culture of approximately 106 CFU/ml to yield concentrations of 0, 0.5, 1, 2, 4, 8, 16, 32, and 64 times the MIC for the strain under study. Subcultures for viable counts were performed on nutrient agar at 0, 5, 10, 15, 20, 25, 30, 45, and 60 min and 2, 3, 4, and 24 h after antibiotic addition. Viable counts were determined after 24 h of incubation of subcultures at 37°C. PAE.[2] The in vitro PAE was determined by the standard in vitro method for two of the three clinical strains noted above and the ATCC strain with both agents. For each experiment, P. aeruginosa (≈106 CFU/ml) in logarithmic phase growth was exposed for 15 min (for colistin) or 1 h (for colistin methanesulfonate) in Mueller-Hinton broth to the antibiotics at concentrations of 0.5, 1, 2, 4, 8, and 16 times the MIC. Fifteen minutes of exposure was used for colistin due to its very rapid bactericidal effect, to ensure that there were adequate numbers of bacteria for sampling at the end of the exposure interval. Antibiotic was removed by twice centrifuging at 3,000 × g for 10 min, decanting the supernatant, and resuspending in prewarmed broth. Viable counts were performed at 0, 1, 2, 3, 4, 5, 6, and 24 h on nutrient agar. A growth control was performed in the same fashion but without exposure to antibiotic. The colonies were counted after 24 h of incubation at 37°C. PAE was determined by comparing regrowth of treated and growth control cultures, using the standard formula of the time for the control culture to increase 10-fold subtracted from the time for the treated culture to do the same. |
| Animal Protocol | Rats: Sterile 0.9% sodium chloride is used to prepare fresh dose solutions of colistin methanesulfonate (sodium) and colistin sulfate. Colistin methanesulfonate (CMS) or sulfate solutions are injected bolus-xstyle through the jugular vein cannula for the intravenous studies. The method for pulmonary administration is called intratracheal (i.t.) instillation. CMS is given intravenously to animals at doses of 14 mg/kg, 28 mg/kg, or 56 mg/kg of body weight. Colistin is given intraperitoneally (i.v.) to rats in an independent study at doses of 0.21 mg/kg, 0.41 mg/kg, or 0.62 mg/kg[3]. |
| Toxicity/Toxicokinetics |
Colistin has no significant genotoxic activity or structural alerts for carcinogenicity, is poorly absorbed from the gastrointestinal tract, and no neoplastic or preneoplastic lesions were observed in 26-week studies in rats given repeated oral or parenteral doses. As such, the Committee concluded that colistin compounds are unlikely to be carcinogenic. The relevant endpoint for risk assessment was determined to be disruption of the colonization barrier in the colon via toxicity to gut flora, the most sensitive organism of which was E. coli, with a minimum inhibitory concentration for 50% of strains (MIC50) of 1 µg colistin base/ml in an in vitro study. The Committee established an ADI of 0–7 µg/kg bw/d (420 µg/p/d for 60-kg adult) on the basis of the MIC50 for E. coli converted to an upper bound ADI value using the following formula: ADI (µg/kg bw/d) = (MIC50 (1 µg/ml) x mass of colonic contents (220 g))/(bioavailable fraction of dose (0.5) x safety factor (1) x bodyweight (60 kg)). The Committee recommended MRLs, measured as colistin A+B, in cattle, sheep, goats, pigs, chickens, turkeys and rabbits of 150 µg/kg liver, muscle and fat (including skin+fat, where applicable), 200 µg/kg in kidney, 300 µg/kg in hens’ eggs, and 50 µg/kg in cows’ and sheep’s milk. The MRLs recommended would result in a TMDI of 229 µg (55% ADI). The calculated EDI values represent 4% (for chickens) to 9% (for cattle) of the upper bound of the ADI. The EDI of 56.9 µg (14% ADI) is calculated using the highest median values from among the tissues and food-producing species. rat LD50 oral 121 mg/kg Antibiotics Annual., 7(61), 1959/1960 rat LD50 intraperitoneal 10572 ug/kg Antibiotics Annual., 7(61), 1959/1960 rat LD50 subcutaneous 72200 ug/kg LUNGS, THORAX, OR RESPIRATION: DYSPNEA; LUNGS, THORAX, OR RESPIRATION: CYANOSIS Kiso to Rinsho. Clinical Report., 13(7), 1979 mouse LD50 oral 793 mg/kg Arzneimittel-Forschung. Drug Research., 11(395), 1961 mouse LD50 intraperitoneal 21800 ug/kg Arzneimittel-Forschung. Drug Research., 11(395), 1961 |
| References |
[1]. Peptide antibiotics. Antimicrob Agents Chemother. 1999 Jun;43(6):1317-23. [2]. In vitro pharmacodynamic properties of colistin and colistin methanesulfonate againstPseudomonas aeruginosa isolates from patients with cystic fibrosis. Antimicrob Agents Chemother. 2001 Mar;45(3):781-5. [3]. Population pharmacokinetics of colistin methanesulfonate in rats: achieving sustained lung concentrations of colistin for targeting respiratory infections. Antimicrob Agents Chemother. 2013 Oct;57(10):5087-95. [4]. Impact of two different colistin dosing strategies on healthy piglet fecal microbiota. Res Vet Sci. 2016 Aug;107:152-60. |
| Additional Infomation |
Colistin Sulfate is cyclic polypeptide antibiotic from Bacillus colistinus. It is composed of Polymyxins E1 and E2 (or Colistins A, B, and C) which act as detergents on cell membranes. Colistin is less toxic than Polymyxin B, but otherwise similar; the methanesulfonate is used orally. The in vitro pharmacodynamic properties of colistin and colistin methanesulfonate were investigated by studying the MICs, time-kill kinetics, and postantibiotic effect (PAE) against mucoid and nonmucoid strains of Pseudomonas aeruginosa isolated from patients with cystic fibrosis. Twenty-three clinical strains, including multiresistant strains, and one type strain were selected for MIC determination. Eleven strains were resistant; MICs for these strains were >128 mg/liter. For the susceptible strains, MICs of colistin ranged from 1 to 4 mg/liter, while the MICs of colistin methanesulfonate were significantly higher and ranged from 4 to 16 mg/liter. The time-kill kinetics were investigated with three strains at drug concentrations ranging from 0.5 to 64 times the MIC. Colistin showed extremely rapid killing, resulting in complete elimination at the highest concentrations within 5 min, while colistin methanesulfonate killed more slowly, requiring a concentration of 16 times the MIC to achieve complete killing within 24 h. Colistin exhibited a significant PAE of 2 to 3 h at 16 times the MIC against the three strains after 15 min of exposure. For colistin methanesulfonate, PAEs were shorter at the concentrations tested. Colistin methanesulfonate had lower overall bactericidal and postantibiotic activities than colistin, even when adjusted for differences in MICs. Our data suggest that doses of colistin methanesulfonate higher than the recommended 2 to 3 mg/kg of body weight every 12 h may be required for the effective treatment of P. aeruginosa infections in cystic fibrosis patients.[2] Colistin is often used in piglets but underdosing and overdosing are frequent. The impact of such administrations on fecal microbiota was studied. Piglets were given either underdoses of colistin by oral gavage for five days or overdoses by in-feed medication for 14days. The composition of fecal microbiota was studied by quantitative PCR, 16S rRNA sequencing, culture of Enterobacteriaceae, and quantification of short-chain fatty acids (SCFAs). The mean colistin concentrations during the treatment for underdosed and overdosed groups were 14.4μg/g and 64.9μg/g of feces respectively. Whatever the piglet and the sampling day, the two main phyla were Firmicutes and Bacteroidetes, The main families were Lactobacillaceae, Clostridiales, Lachnospiraceae and Ruminococcaceae. The main perturbation was the significant but transitory decrease in the Escherichia coli population during treatment, yet all the E. coli isolates were susceptible to colistin. Moreover, colistin did not affect the production of SCFAs. These results show that under- or overdoses of colistin do not result in any major disturbance of piglet fecal microbiota and rarely select for chromosomal resistance in the dominant E. coli population.[4] |
Solubility Data
| Solubility (In Vitro) | H2O : ~50 mg/mL (~35.70 mM) |
| Solubility (In Vivo) |
Solubility in Formulation 1: 50 mg/mL (35.70 mM) in PBS (add these co-solvents sequentially from left to right, and one by one), clear solution; with sonication. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 0.7140 mL | 3.5698 mL | 7.1396 mL | |
| 5 mM | 0.1428 mL | 0.7140 mL | 1.4279 mL | |
| 10 mM | 0.0714 mL | 0.3570 mL | 0.7140 mL |