Physicochemical Properties
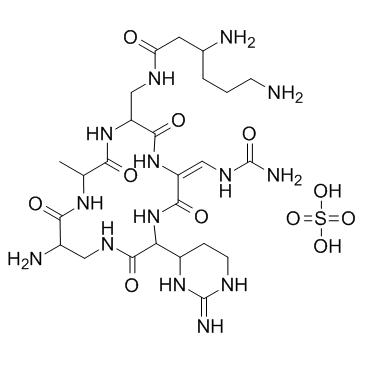
| Molecular Formula | C25H48N14O16S2 |
| Molecular Weight | 864.861 |
| Exact Mass | 752.298 |
| Elemental Analysis | C, 39.57; H, 6.11; N, 25.84; O, 24.25; S, 4.23 |
| CAS # | 1405-37-4 |
| Related CAS # | Capreomycin;11003-38-6 |
| PubChem CID | 134071939 |
| Appearance | White to off-white solid powder |
| Boiling Point | 1376.7ºC at 760mmHg |
| Flash Point | 786.4ºC |
| Vapour Pressure | 0mmHg at 25°C |
| Hydrogen Bond Donor Count | 16 |
| Hydrogen Bond Acceptor Count | 16 |
| Rotatable Bond Count | 9 |
| Heavy Atom Count | 51 |
| Complexity | 1310 |
| Defined Atom Stereocenter Count | 3 |
| SMILES | S(=O)(=O)(O[H])O[H].O=C1C([H])(C2([H])C([H])([H])C([H])([H])N=C(N([H])[H])N2[H])N([H])C(/C(=C(\[H])/N([H])C(N([H])[H])=O)/N([H])C([C@]([H])(C([H])([H])N([H])C([C@]([H])(C([H])([H])C([H])([H])C([H])([H])N([H])[H])N([H])[H])=O)N([H])C(C([H])(C([H])([H])O[H])N([H])C([C@]([H])(C([H])([H])N1[H])N([H])[H])=O)=O)=O)=O |
| InChi Key | TUATYNXRYJTQTQ-RIQUSILOSA-N |
| InChi Code | InChI=1S/C25H44N14O8.C25H44N14O7.2H2O4S/c26-4-1-2-11(27)6-17(41)32-8-14-20(43)35-15(9-34-25(30)47)21(44)39-18(13-3-5-31-24(29)38-13)23(46)33-7-12(28)19(42)37-16(10-40)22(45)36-14;1-11-19(41)36-15(9-32-17(40)7-12(27)3-2-5-26)21(43)37-16(10-34-25(30)46)22(44)39-18(14-4-6-31-24(29)38-14)23(45)33-8-13(28)20(42)35-11;2*1-5(2,3)4/h9,11-14,16,18,40H,1-8,10,26-28H2,(H,32,41)(H,33,46)(H,35,43)(H,36,45)(H,37,42)(H,39,44)(H3,29,31,38)(H3,30,34,47);10-15,18H,2-9,26-28H2,1H3,(H,32,40)(H,33,45)(H,35,42)(H,36,41)(H,37,43)(H,39,44)(H3,29,31,38)(H3,30,34,46);2*(H2,1,2,3,4)/b15-9+;16-10+;;/t11-,12-,13+,14-,16-,18-;11-,12-,13-,14+,15-,18-;;/m00../s1 |
| Chemical Name | sulfuric acid compound with (S)-3,6-diamino-N-(((2S,5S,11S,15S,E)-15-amino-11-((R)-2-amino-3,4,5,6-tetrahydropyrimidin-4-yl)-2-(hydroxymethyl)-3,6,9,12,16-pentaoxo-8-(ureidomethylene)-1,4,7,10,13-pentaazacyclohexadecan-5-yl)methyl)hexanamide and (S)-3,6-diamino-N-(((2S,5S,11S,15S,E)-15-amino-11-((R)-2-amino-3,4,5,6-tetrahydropyrimidin-4-yl)-2-methyl-3,6,9,12,16-pentaoxo-8-(ureidomethylene)-1,4,7,10,13-pentaazacyclohexadecan-5-yl)methyl)hexanamide (1:1:1) |
| Synonyms | Capreomycin Sulfate; Kapreomycin; Capostatin; |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month Note: Please store this product in a sealed and protected environment, avoid exposure to moisture. |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | Aminoglycoside |
| ln Vitro | The cyclic peptide antibiotics capreomycin and viomycin are generally effective against the bacterial pathogen Mycobacterium tuberculosis. However, recent virulent isolates have become resistant by inactivation of their tlyA gene. We show here that tlyA encodes a 2'-O-methyltransferase that modifies nucleotide C1409 in helix 44 of 16S rRNA and nucleotide C1920 in helix 69 of 23S rRNA. Loss of these previously unidentified rRNA methylations confers resistance to capreomycin and viomycin. Many bacterial genera including enterobacteria lack a tlyA gene and the ensuing methylations and are less susceptible than mycobacteria to capreomycin and viomycin. We show that expression of recombinant tlyA in Escherichia coli markedly increases susceptibility to these drugs. When the ribosomal subunits associate during translation, the two tlyA-encoded methylations are brought into close proximity at interbridge B2a. The location of these methylations indicates the binding site and inhibitory mechanism of capreomycin and viomycin at the ribosome subunit interface[1]. |
| ln Vivo | Capreomycin is used for the treatment of multidrug-resistant tuberculosis (MDR-TB), but it is limited therapeutically by its severe side effects. The objectives of the present studies were (i) to design low-density porous capreomycin sulfate particles for efficient pulmonary delivery to improve local and systemic drug bioavailability and capacity to reduce the bacillary load in the lungs in a manner similar to that achieved with intramuscular injections; (ii) to determine pharmacokinetic parameters after pulmonary administration of these capreomycin particles; and (iii) to evaluate the efficacy of these particles in treating animals in a small-aerosol-inoculum guinea pig model of TB. Capreomycin particles were manufactured by spray drying and characterized in terms of size and drug content. Pharmacokinetic parameters were determined by noncompartmental methods with healthy guinea pigs after administration of capreomycin particles by insufflation. The efficacy of the particles was evaluated by histopathological analysis and in terms of wet organ weight and bacterial burden in TB-infected animals. Lungs of animals receiving a 14.5-mg/kg dose of capreomycin particles showed significantly lower wet weights and smaller bacterial burdens than those of animals receiving any other treatment. These results were supported by histopathological analysis. The feasibility of inhaling capreomycin in a novel powder form, with the ultimate objective of the treatment of MDR-TB, is demonstrated by pharmacokinetic and pharmacodynamic studies with guinea pigs. If applied to humans with MDR-TB, such a therapeutic approach might simplify drug delivery by eliminating injections and might reduce adverse effects through lowering the dose[3]. |
| Enzyme Assay |
M. tuberculosis wild-type Beijing D3 and rrl mutant C-401 were inoculated in triplicate into 7H9 media without drug and 7H9 media containing 10 μg/ml capreomycin and were grown at 37°C for 21 days. Growth of the cultures was monitored daily at OD600. The MICs of antibiotics were determined for each strain as previously described (Maus et al., 2005a, Maus et al., 2005b).[1] Overnight cultures of E. coli cells were diluted 105-fold and plated onto Lauria-Bertani agar (Sambrook et al., 1989) containing viomycin, capreomycin, kanamycin, or rifampicin with concentrations increasing in 2-fold steps. The agar plates were incubated at 37°C, and MICs were scored as the lowest concentration at which no growth was observed.[1] |
| Animal Protocol |
Pharmacokinetic (PK) studies.[3] Animals were randomly divided into five groups receiving capreomycin as follows: intravenously (i.v.; n = 6) and i.m. (n = 8) in solution at a dose of 20 mg/kg and as dry powder insufflated by the pulmonary route at low (n = 6), medium (n = 6), and high (n = 8) nominal doses of 1.4, 7.2, and 14.5 mg/kg. These doses were based on the dose reduction estimated from direct delivery of antibiotics to the lungs by insufflation (circumventing oropharyngeal deposition) and on the practical limitations of easily delivering large masses of dry powders to the guinea pigs. Blood samples (0.35 ml) were collected from each animal into heparinized tubes at 0, 0.08, 0.25, 0.5, 1.0, 1.5, 2, 3, 4, 5, 6, 8, and 12 h. After collection of the last blood sample, animals were euthanized by exsanguination and bronchoalveolar lavage (BAL) was conducted (5 ml sterile saline). Pharmacodynamic studies.3] Animals were infected via the respiratory route with nebulized suspensions (2 × 105 CFU/ml) of Mycobacterium tuberculosis (strain H37Rv), employing an aerosol exposure chamber. Animals remained untreated until 4 weeks following infection, when the bacterial burden is known to plateau. Animals were then assigned to different groups of six guinea pigs each to receive capreomycin daily for 4 weeks by i.m. injection or by inhalation using a custom-designed dry powder dosing chamber. |
| References |
[1]. Capreomycin binds across the ribosomal subunit interface using tlyA-encoded 2'-O-methylations in 16S and 23S rRNAs. Mol Cell. 2006 Jul 21;23(2):173-82. [2]. Mutation of tlyA confers capreomycin resistance in Mycobacterium tuberculosis. Antimicrob Agents Chemother. 2005 Feb;49(2):571-7.[3]. Inhaled large porous particles of capreomycin for treatment of tuberculosis in a guinea pig model. Antimicrob Agents Chemother. 2007 Aug;51(8):2830-6. |
| Additional Infomation | Capreomycin, an important drug for the treatment of multidrug-resistant tuberculosis, is a macrocyclic peptide antibiotic produced by Saccharothrix mutabolis subspecies capreolus. The basis of resistance to this drug was investigated by isolating and characterizing capreomycin-resistant strains of Mycobacterium smegmatis and Mycobacterium tuberculosis. Colonies resistant to capreomycin were recovered from a library of transposon-mutagenized M. smegmatis. The transposon insertion site of one mutant was mapped to an open reading frame in the unfinished M. smegmatis genome corresponding to the tlyA gene (Rv1694) in the M. tuberculosis H37Rv genome. In M. smegmatis spontaneous capreomycin-resistant mutants, the tlyA gene was disrupted by one of three different naturally occurring insertion elements. Genomic DNAs from pools of transposon mutants of M. tuberculosis H37Rv were screened by PCR by using primers to the tlyA gene and the transposon to detect mutants with an insertion in the tlyA gene. One capreomycin-resistant mutant was recovered that contained the transposon inserted at base 644 of the tlyA gene. Complementation with the wild-type tlyA gene restored susceptibility to capreomycin in the M. smegmatis and M. tuberculosis tlyA transposon mutants. Mutations were found in the tlyA genes of 28 spontaneous capreomycin-resistant mutants generated from three different M. tuberculosis strains and in the tlyA genes of capreomycin-resistant clinical isolates. In in vitro transcription-translation assays, ribosomes from tlyA mutant but not tlyA(+) strains resist capreomycin inhibition of transcription-translation. Therefore, TlyA appears to affect the ribosome, and mutation of tlyA confers capreomycin resistance[2]. |
Solubility Data
| Solubility (In Vitro) | H2O : ≥ 37 mg/mL (~49.28 mM) |
| Solubility (In Vivo) |
Solubility in Formulation 1: 100 mg/mL (133.19 mM) in PBS (add these co-solvents sequentially from left to right, and one by one), clear solution; with sonication. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.1563 mL | 5.7813 mL | 11.5626 mL | |
| 5 mM | 0.2313 mL | 1.1563 mL | 2.3125 mL | |
| 10 mM | 0.1156 mL | 0.5781 mL | 1.1563 mL |