Physicochemical Properties
| Molecular Formula | C17H17CL2N3 |
| Molecular Weight | 334.242981672287 |
| Exact Mass | 333.079 |
| CAS # | 912780-51-9 |
| PubChem CID | 6621371 |
| Appearance | White to off-white solid powder |
| Density | 1.3±0.1 g/cm3 |
| Boiling Point | 499.1±55.0 °C at 760 mmHg |
| Flash Point | 255.6±31.5 °C |
| Vapour Pressure | 0.0±1.3 mmHg at 25°C |
| Index of Refraction | 1.632 |
| LogP | 4.62 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 2 |
| Rotatable Bond Count | 5 |
| Heavy Atom Count | 22 |
| Complexity | 355 |
| Defined Atom Stereocenter Count | 0 |
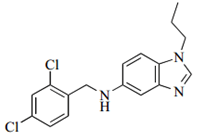
| SMILES | ClC1C=C(Cl)C(CNC2C=C3N=CN(C3=CC=2)CCC)=CC=1 |
| InChi Key | PWEPSIFNTIQCNN-UHFFFAOYSA-N |
| InChi Code | InChI=1S/C17H17Cl2N3/c1-2-7-22-11-21-16-9-14(5-6-17(16)22)20-10-12-3-4-13(18)8-15(12)19/h3-6,8-9,11,20H,2,7,10H2,1H3 |
| Chemical Name | N-[(2,4-dichlorophenyl)methyl]-1-propylbenzimidazol-5-amine |
| Synonyms | 912780-51-9; N-[(2,4-dichlorophenyl)methyl]-1-propylbenzimidazol-5-amine; MmpL3 inhibitor C215; C-215; N-(2,4-dichlorobenzyl)-1-propyl-1H-benzimidazol-5-amine; C215; N-(2,4-Dichlorobenzyl)-1-propyl-1H-benzo[d]imidazol-5-amine; |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | Mycobacterial membrane protein large 3 (MmpL3); M. tuberculosis (IC90 = 16 μM) |
| ln Vitro | C215 (N-(2,4-dichlorobenzyl)-1-propyl-1H-benzo[d]imidazol-5-amine) is an inhibitor (Figure 4a) that we identified in HTS with glycerol independent activity against M. tuberculosis, limited non-specific toxicity against mammalian cells, an IC90 of 16μM against M. tuberculosis, and efficacy against M. tuberculosis growing in macrophages (Table S1, Table S2, compound 72). Four independent resistant mutants were generated to C215 . These mutants had IC90 values that were shifted only ~2 fold relative to the wild-type parents used for resistance generation (Figure 4b). Sequencing of the genomes of the four resistant mutants identified Rv0206c as the only gene with mutations identified in all four resistant mutants, suggesting that mutation of Rv0206c confers resistance to C215. Rv0206c MmpL3, a member of the resistance, nodulation and cell division (RND) family of proteins that are thought to encode lipid transporters in M. tuberculosis. AU12345, a recently identified adamantyl urea compound with activity against M. tuberculosis, targets MmpL3, resulting in inhibition of the transport of mycolic acids across the inner membrane. In addition, SQ109, a 1,2-diamine related to ethambutol, was also shown to target MmpL3. These compounds were used to demonstrate that MmpL3 encodes a transporter of trehalose-monomycolate (TDM), an essential precursor to myolic acid containing lipid species in the outer mycolate membrane. The target of AU12345 was identified using the method of resistance generation coupled to genome sequencing, and resistant mutants were found to harbor a single mutation in mmpL3 (G758A). In contrast, in our analysis of C215 resistant mutants, a different mutation in mmpL3 was identified in each of the resistant mutants we isolated (L320P, T667A, V684A, V51A). To demonstrate that C215 kills M. tuberculosis by inhibiting MmpL3 and transport of mycolic acids across the inner membrane, we treated cells with 1x, 5x, and 10x the MIC of C215, and examined cell wall mycolic acids. We observed a dose dependent decrease in cell wall bound mycolic acids (α, methoxy, and keto) upon treatment with C215, similar to the effect previously reported for AU12345, confirming that MmpL3 is the likely target of C215. This represents the fourth identification of a small molecule that kills M. tuberculosis by inhibiting MmpL3 [1]. |
| Enzyme Assay |
Screening, hit selection, and IC90 determinations [1] For M. tuberculosis and BCG screening assays, bacteria expressing GFP was grown to mid-log phase (OD600=0.6–0.8), diluted, and plated into 384 well plates into which compounds had previously been pinned for a final OD600 of 0.025 and compound concentration of 25μM or 20μg mL−1 (NIH inhibitors). Plates were incubated for a period of 72h, at which time GFP fluorescence was read. Each compound was screened in duplicate, and composite z-scores were calculated using DMSO controls as reference. Hits from the M. tuberculosis screen were defined as compounds with a composite z-score of less than −4. This z-score cutoff was selected using average of the z-scores of the concentrations of the control antibiotics clofazimine and rifampicin that gave a Z′-factor of 0, meaning that the distance separating the positive and negative controls is 3x the sum of the standard deviations of the two populations. For dose response curves and IC90 determination of hits from the screens, bacteria were grown to mid-log phase and plated in 96 well plates at OD600=0.05 in the presence of small molecule inhibitors for 7 days unless otherwise indicated, and growth was assessed by reading OD600. The IC90 was defined as the minimum concentration that inhibited growth by 90% relative to the DMSO control. For the M. smegmatis screen, OD600 was used as the readout and the plates were read after 2 days of incubation. Secondary Screening Assays [1] Hits from the primary screen against M. tuberculosis were cherry picked from the library and arrayed in 384 well plates as a dose response curve using 2 fold serial dilutions from the primary screening concentration. Preliminary cherrypick plate MIC values were determined using the GFP based assay and are reported as the minimum concentration that gives the maximum inhibition observed using rifampicin controls. Macrophage activity was assessed by infecting J774 macrophages plated into 96 well plates with a strain of M. tuberculosis constitutively expressing firefly luciferase. After three days of infection in the presence of inhibitors, the infected monolayers were washed, lysed, and luminescence was used as a reporter of bacterial viability. To determine macrophage toxicity, J774 macrophages were incubated with small molecules for a period of 3 days upon which time CellTiter-Glo was used as a readout for macrophage viability. |
| Cell Assay |
Generation of resistant mutants [1] The MIC of each compound on solid media was identified by plating 107 bacteria on agar containing a dose response in 96 well plate format. The MIC was defined as the lowest concentration resulting in inhibition of bacterial growth. Resistant mutants were generated by plating M. tuberculosis cells onto agar pads containing 2x and 10x the agar MIC of each compound using four independently derived wild-type clones. Colonies that arose on inhibitor containing plates were inoculated into liquid media containing 1x the liquid MIC of the inhibitor. These cultures were grown to mid-log and samples were retested in a liquid MIC assay to confirm that a shift relative to the wild-type MIC was observed. Metabolic labeling of mycolic acids and compound treatment [1] 10mL cultures of M. tuberculosis were grown to OD600=0.6 in inkwell bottles. 1x, 5x, or 10x the MIC of C215 added to the cultures simultaneously with 10μCi of 14C acetate. After 20h of labeling, the cultures were washed once with water, saponified with tetrabutylammonium hydroxide, and methyl esters of fatty acids and mycolic acids created by addition of methyl iodide. Fatty acid methyl esters (FAMEs) and mycolic acid methyl esters (MAMEs) were extracted from the aqueous layer using methylene chloride, and run out on TLC plates using 95:5 hexanes:ethyl acetate. TLC plates were loading was normalized according to the OD600 of the cells after the 20h treatment period. FAMEs and MAMEs were visualized by phosphorimaging. |
| References | [1]. Identification of novel inhibitors of M. tuberculosis growth using whole cell based high-throughput screening. ACS Chem Biol. 2012;7(8):1377-1384. |
| Additional Infomation |
Despite the urgent need for new antitubercular drugs, few are on the horizon. To combat the problem of emerging drug resistance, structurally unique chemical entities that inhibit new targets will be required. Here we describe our investigations using whole cell screening of a diverse collection of small molecules as a methodology for identifying novel inhibitors that target new pathways for Mycobacterium tuberculosis drug discovery. We find that conducting primary screens using model mycobacterial species may limit the potential for identifying new inhibitors with efficacy against M. tuberculosis. In addition, we confirm the importance of developing in vitro assay conditions that are reflective of in vivo biology for maximizing the proportion of hits from whole cell screening that are likely to have activity in vivo. Finally, we describe the identification and characterization of two novel inhibitors that target steps in M. tuberculosis cell wall biosynthesis. The first is a novel benzimidazole that targets mycobacterial membrane protein large 3 (MmpL3), a proposed transporter for cell wall mycolic acids. The second is a nitro-triazole that inhibits decaprenylphosphoryl-β-D-ribose 2'-epimerase (DprE1), an epimerase required for cell wall biosynthesis. These proteins are both among the small number of new targets that have been identified by forward chemical genetics using resistance generation coupled with genome sequencing. This suggests that methodologies currently employed for screening and target identification may lead to a bias in target discovery and that alternative methods should be explored. [1] All currently used antibiotics were discovered using whole cell screening, highlighting the importance of this approach. In this report we describe our experiences with whole cell high-throughput screening to identify novel inhibitors of M. tuberculosis replication using both an unbiased collection of >20K compounds from the Broad Institute and a set of 1113 hit compounds made available to the M. tuberculosis screening community by the NIAID. This latter data set provides independent verification and testing of the NIAID compounds to help define the importance of this collection to M. tuberculosis drug discovery efforts. In addition, by analyzing the primary and secondary screening data from the Broad collection, we were able to expand upon and quantify observations related to whole cell screening. This study using a large compound collection with no predicted potential for structural bias found an even smaller degree of overlap in compounds then previously reported (14) that are active against three mycobacterial species, clearly demonstrating the potential pitfalls of using surrogate mycobacterial species for identifying inhibitors of M. tuberculosis growth. In addition, this work describes the surprisingly high rate at which such hits are identified from whole cell screening that bear the recognized characteristic of dependence on growth on standard glycerol containing M. tuberculosis media. This is particularly important, as inhibitors of this nature have no potential for in vivo activity, suggesting that a major shift away from the standard growth media used for the study of M. tuberculosis may be warranted, particularly with respect to chemical biological investigations. Finally, we note the interesting phenomenon of repeated identification of the same targets DprE1 and Mmpl3 by the methods utilized, which may suggest that they are highly targetable but also raise the caveat that they may be targets that are easily mutated to confer resistance. In summary, this work provides insights and perspectives that should help guide future M. tuberculosis screening efforts and antibiotic discovery in general. [1] |
Solubility Data
| Solubility (In Vitro) | May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples |
| Solubility (In Vivo) |
Note: Listed below are some common formulations that may be used to formulate products with low water solubility (e.g. < 1 mg/mL), you may test these formulations using a minute amount of products to avoid loss of samples. Injection Formulations (e.g. IP/IV/IM/SC) Injection Formulation 1: DMSO : Tween 80: Saline = 10 : 5 : 85 (i.e. 100 μL DMSO stock solution → 50 μL Tween 80 → 850 μL Saline) *Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH ₂ O to obtain a clear solution. Injection Formulation 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL DMSO → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Injection Formulation 3: DMSO : Corn oil = 10 : 90 (i.e. 100 μL DMSO → 900 μL Corn oil) Example: Take the Injection Formulation 3 (DMSO : Corn oil = 10 : 90) as an example, if 1 mL of 2.5 mg/mL working solution is to be prepared, you can take 100 μL 25 mg/mL DMSO stock solution and add to 900 μL corn oil, mix well to obtain a clear or suspension solution (2.5 mg/mL, ready for use in animals). Injection Formulation 4: DMSO : 20% SBE-β-CD in saline = 10 : 90 [i.e. 100 μL DMSO → 900 μL (20% SBE-β-CD in saline)] *Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Injection Formulation 5: 2-Hydroxypropyl-β-cyclodextrin : Saline = 50 : 50 (i.e. 500 μL 2-Hydroxypropyl-β-cyclodextrin → 500 μL Saline) Injection Formulation 6: DMSO : PEG300 : castor oil : Saline = 5 : 10 : 20 : 65 (i.e. 50 μL DMSO → 100 μLPEG300 → 200 μL castor oil → 650 μL Saline) Injection Formulation 7: Ethanol : Cremophor : Saline = 10: 10 : 80 (i.e. 100 μL Ethanol → 100 μL Cremophor → 800 μL Saline) Injection Formulation 8: Dissolve in Cremophor/Ethanol (50 : 50), then diluted by Saline Injection Formulation 9: EtOH : Corn oil = 10 : 90 (i.e. 100 μL EtOH → 900 μL Corn oil) Injection Formulation 10: EtOH : PEG300:Tween 80 : Saline = 10 : 40 : 5 : 45 (i.e. 100 μL EtOH → 400 μLPEG300 → 50 μL Tween 80 → 450 μL Saline) Oral Formulations Oral Formulation 1: Suspend in 0.5% CMC Na (carboxymethylcellulose sodium) Oral Formulation 2: Suspend in 0.5% Carboxymethyl cellulose Example: Take the Oral Formulation 1 (Suspend in 0.5% CMC Na) as an example, if 100 mL of 2.5 mg/mL working solution is to be prepared, you can first prepare 0.5% CMC Na solution by measuring 0.5 g CMC Na and dissolve it in 100 mL ddH2O to obtain a clear solution; then add 250 mg of the product to 100 mL 0.5% CMC Na solution, to make the suspension solution (2.5 mg/mL, ready for use in animals). Oral Formulation 3: Dissolved in PEG400 Oral Formulation 4: Suspend in 0.2% Carboxymethyl cellulose Oral Formulation 5: Dissolve in 0.25% Tween 80 and 0.5% Carboxymethyl cellulose Oral Formulation 6: Mixing with food powders Note: Please be aware that the above formulations are for reference only. InvivoChem strongly recommends customers to read literature methods/protocols carefully before determining which formulation you should use for in vivo studies, as different compounds have different solubility properties and have to be formulated differently. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.9919 mL | 14.9593 mL | 29.9186 mL | |
| 5 mM | 0.5984 mL | 2.9919 mL | 5.9837 mL | |
| 10 mM | 0.2992 mL | 1.4959 mL | 2.9919 mL |