Amphotericin B (Fungizone; Amfocan; Ambisome; NSC527017; Amphozone; Fungilin; Amfocare; Amfotex; Amfotex) is a naturally occurring polyene antifungal agent approved for treating serious fungal infections and leishmaniasis, such as mucormycosis, coccidioidomycosis, candidiasis, aspergillosis, blastomycosis, and cryptococcosis.
Physicochemical Properties
| Exact Mass | 923.487 |
| Elemental Analysis | C, 61.09; H, 7.96; N, 1.52; O, 29.43 |
| CAS # | 1397-89-3 |
| Related CAS # | Amphotericin B trihydrate;1202017-46-6;Amphotericin B-13C6 |
| PubChem CID | 5280965 |
| Appearance | Light yellow to yellow solid |
| Density | 1.3±0.1 g/cm3 |
| Boiling Point | 1140.4±65.0 °C at 760 mmHg |
| Melting Point | >170°C |
| Flash Point | 643.5±34.3 °C |
| Vapour Pressure | 0.0±0.6 mmHg at 25°C |
| Index of Refraction | 1.614 |
| LogP | 1.16 |
| Hydrogen Bond Donor Count | 12 |
| Hydrogen Bond Acceptor Count | 18 |
| Rotatable Bond Count | 3 |
| Heavy Atom Count | 65 |
| Complexity | 1670 |
| Defined Atom Stereocenter Count | 19 |
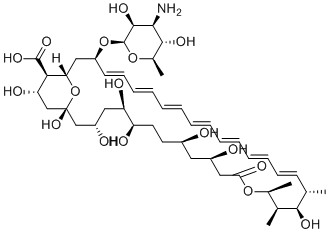
| SMILES | C[C@H]1/C=C/C=C/C=C/C=C/C=C/C=C/C=C/[C@@H](C[C@H]2[C@@H]([C@H](C[C@](O2)(C[C@H](C[C@H]([C@@H](CC[C@H](C[C@H](CC(=O)O[C@H]([C@@H]([C@@H]1O)C)C)O)O)O)O)O)O)O)C(=O)O)O[C@H]3[C@H]([C@H]([C@@H]([C@H](O3)C)O)N)O |
| InChi Key | APKFDSVGJQXUKY-INPOYWNPSA-N |
| InChi Code | InChI=1S/C47H73NO17/c1-27-17-15-13-11-9-7-5-6-8-10-12-14-16-18-34(64-46-44(58)41(48)43(57)30(4)63-46)24-38-40(45(59)60)37(54)26-47(61,65-38)25-33(51)22-36(53)35(52)20-19-31(49)21-32(50)23-39(55)62-29(3)28(2)42(27)56/h5-18,27-38,40-44,46,49-54,56-58,61H,19-26,48H2,1-4H3,(H,59,60)/b6-5+,9-7+,10-8+,13-11+,14-12+,17-15+,18-16+/t27-,28-,29-,30+,31+,32+,33-,34-,35+,36+,37-,38-,40+,41-,42+,43+,44-,46-,47+/m0/s1 |
| Chemical Name | (1R,3S,5R,6R,9R,11R,15S,16R,17R,18S,19E,21E,23E,25E,27E,29E,31E,33R,35S,36R,37S)-33-(((2R,3S,4S,5S,6R)-4-amino-3,5-dihydroxy-6-methyltetrahydro-2H-pyran-2-yl)oxy)-1,3,5,6,9,11,17,37-octahydroxy-15,16,18-trimethyl-13-oxo-14,39-dioxabicyclo[33.3.1]nonatriaconta-19,21,23,25,27,29,31-heptaene-36-carboxylic acid |
| Synonyms | Amphotericin B;NSC 527017;Ambisome NSC527017;Amphozone FungilinFungizoneAMPH-B Fungizone Liposomal Amphotericin B NSC-527017 |
| HS Tariff Code | 2934.99.9001 |
| Storage |
Powder-20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month Note: This product requires protection from light (avoid light exposure) during transportation and storage. |
| Shipping Condition | Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs) |
Biological Activity
| Targets | Leishmania;Plasmodium |
| ln Vitro | The infusion-related toxicity of amphotericin B, which includes fever and chills, limits its administration. This effect is thought to be caused by innate immune cells producing proinflammatory cytokines. TLR2 and CD14-expressing cells release inflammatory cytokines and undergo signal transduction when exposed to amphotericin B[1]. Amphotericin B's relative toxicity limits its usefulness as it interacts with cholesterol, the primary sterol found in mammalian membranes. In the subphase, amphotericin B is distributed either as a highly aggregated state or as a pre-micellar state[2].Amphotericin B only kills Leishmania promastigotes (LPs) that are unicellular when they form aqueous pores that are permeable to small cations and anions. A polarization potential is induced by amphotericin B (0.1 mM) in liposomes loaded with KCl and suspended in an iso-osmotic sucrose solution, signifying K+ leakage. The negative membrane potential nearly completely collapses when amphotericin B (0.05 mM) is added, indicating Na+ entry into the cells[3]. |
| ln Vivo | In the hamster scrapie model, amphotericin B causes the incubation period to be extended and the accumulation of PrPSc to be reduced. In mice suffering from transmissible subacute spongiform encephalopathies (TSSE), amphotericin B significantly lowers PrPSc levels[4]. In mouse malaria, amphotericin B directly affects Plasmodium falciparum and has an impact on parasitemia, host survival, and eryptosis of infected erythrocytes. In mice infected with Plasmodium berghei, amphotericin B tends to postpone the development of parasitemia and considerably postpones host death[5]. |
| Enzyme Assay | Polyfect reagent and DEAE-dextran are used to transiently transfect THP-1 and HEK293 cells, respectively. Genes encoding the NF-κB-dependent pELAM-luc luciferase reporter, TLR2, TLR4, CD14, and MD2 are present in transfected plasmids. In 12-well plates, cells (5×105 THP-1 or 1×105 HEK293) are added, and after 18 hours, they are washed and stimulated for 5 hours. Following the instructions, cells are lysed in reporter lysis buffer, and the lysates are subjected to luminescence analysis using a Monolight 3010 luminometer and Promega luciferase substrate. |
| Cell Assay | AmB-induced cell death kinetics against Leishmania promastigotes are monitored via fluorometry employing ethidium bromide (EB), a compound that binds DNA. A SPEX Fluorolog II spectrophotometer is used to measure fluorescence at excitation-emission wavelengths of 365–580 nm. Promastigotes are added to a fluorescence cuvette containing 2 mL of various buffered solutions, always containing 10 mM glucose and 50 mM EB, and incubated for 5 minutes with gentle stirring at a final concentration of 25×106 cells/mL.Following the attainment of signal stabilization, AmB is introduced and dissolved in dimethylsulfoxide. Digitonin (50 mg/mL) is always added to achieve maximum EB incorporation. A buffer of 75 mM TRIS (pH 4 7.6) is applied to all solutions, which also contain 150 mM KCl (BK+), 150 mM NaCl (BNa+), 150 mM choline chloride, 100 mM sucrose, and 100 mM NaCl. A sophisticated instrument called the SW2 osmometer is always used to adjust the osmolarity of all solutions to 390±5 mOsm. |
| Animal Protocol |
Efficacy of PEO-b-p(HASA)/AmB. Efficacy was assessed by organism killing in the kidneys of a neutropenic murine model of disseminated fungal infection as described previously by Andes et al. A clinical isolate of Candida albicans (K-1) was grown and quantified on SDA. For 24 h prior to infection, the organism was subcultured at 35 °C on SDA slants. A 106 CFU/mL inoculum (CFU, colony forming units) was prepared by placing six fungal colonies into 5 mL of sterile, depyrogenated normal (0.9%) saline warmed to 35 °C. Six-week-old ICR/Swiss specific-pathogen-free female mice were obtained from Harlan Sprague Dawley . All animal studies were approved by the Animal Research Committee of the William S. Middleton Memorial VA Hospital (Madison, WI). The mice were weighed (23−27 g) and given intraperitoneal injections of cyclophosphamide to render neutropenia. (For the purposes of this study, neutropenia was defined as <100 polymorphonuclear leukocytes/mm3.) Each mouse was dosed with 150 mg/kg of cyclophosphamide 4 days prior to infection and 100 mg/kg 1 day before infection. Disseminated candidiasis was induced via tail vein injection of 100 μL of inoculum. [5] The AmB/polymeric micelle formulations or micelle blanks were reconstituted with 1.0 mL of 5% dextrose. The treatment group was given single 200 μL intravenous (iv) injections of reconstituted AmB/PEO-b-p(HASA), 91% 2 h postinfection. Doses were calculated in terms of mg of AmB/kg of body weight. Control animals were given a placebo of “blank” polymeric micelles. Over time, two animals per experimental condition were sacrificed by CO2 asphyxiation. The kidneys from each animal were removed and homogenized. The homogenate was diluted 10-fold with 9% saline and plated on SDA. The plates were then incubated for 24 h at 35 °C and inspected for CFU determination. The lower limit of detection for this technique is 100 CFU/mL. To compare the antifungal activity of the AmB/ micelle formulations with that of Fungizone, animals were dosed with equivalent doses of AmB as Fungizone as described above. The control animals for the Fungizone group received 200 μL iv injections of 5% dextrose. All results are expressed as the mean CFU per kidney for two animals (four kidneys total). The change in the area under the time−kill curves was calculated by ΔAUCTK = AUCcontrol − AUCtreatment. Outcomes were compared using ANOVA on ranks.[5] |
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion Bioavailability is 100% for intravenous infusion. 39 +/- 22 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 1 mg/kg/day at Day 1] 17 +/- 6 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 1 mg/kg/day 3-20 days later] 51 +/- 44 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 2.5 mg/kg/day at Day 1] 22 +/- 15 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 2.5 mg/kg/day 3-20 days later] 21 +/- 14 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 5 mg/kg/day at Day 1] 11 +/- 6 mL/hr/kg [febrile neutropenic cancer and bone marrow transplant patients receiving infusion of 5 mg/kg/day 3-20 days later] The pharmacokinetics of amphotericin B vary substantially depending on whether the drug is administered as conventional amphotericin B (formulated with sodium desoxycholate), amphotericin B cholesteryl sulfate complex, amphotericin B lipid complex, or amphotericin B liposomal, and pharmacokinetic parameters reported for one amphotericin B formulation should not be used to predict the pharmacokinetics of any other amphotericin B formulation. Amphotericin B is poorly absorbed from the GI tract and must be given parenterally to treat systemic fungal infections. In one study, immediately after completion of iv infusion of 30 mg of amphotericin B (administered over a period of several hours), average peak serum concentrations were about 1 ug/ml; when the dose was 50 mg, average peak serum concentrations were approximately 2 ug/ml. Immediately after infusion, no more than 10% of the amphotericin B dose can be accounted for in serum. Average minimum serum concentrations (recorded just prior to the next drug infusion) of approximately 0.4 ug/ml have been reported when doses of 30 mg were given daily or when doses of 60 mg were given every other day. Information on the distribution of amphotericin B is limited, although distribution is apparently multicompartmental. The volume of distribution of the drug following administration of conventional amphotericin B has been reported to be 4 L/kg; the volume of distribution at steady state after administration of amphotericin B cholesteryl sulfate is reported to be 3.8-4.1 L/kg. Amphotericin B concentrations attained in inflamed pleura, peritoneum, synovium, and aqueous humor following IV administration of conventional amphotericin B reportedly are about 60% of concurrent plasma concentrations; the drug also is distributed into vitreous humor, pleural, pericardial, peritoneal, and synovial fluid. Amphotericin B reportedly crosses the placenta and low concentrations are attained in amniotic fluid. Following IV administration of conventional amphotericin B, CSF concentrations of the drug are approximately 3% of concurrent serum concentrations. To achieve fungistatic CSF concentrations, the drug must usually be administered intrathecally. In patients with meningitis, intrathecal administration of 0.2-0.3 mg of conventional amphotericin B via a subcutaneous reservoir has produced peak CSF concentrations of 0.5-0.8 ug/mL; 24 hours after the dose, CSF concentrations were 0.11-0.29 ug/mL. Amphotericin B is removed from the CSF by arachnoid villi and appears to be stored in the extracellular compartment of the brain, which may act as a reservoir for the drug. For more Absorption, Distribution and Excretion (Complete) data for AMPHOTERICIN B (14 total), please visit the HSDB record page. Metabolism / Metabolites Exclusively renal Biological Half-Life An elimination half-life of approximately 15 days follows an initial plasma half-life of about 24 hours. Amphotericin B cholesteryl sulfate complex has a distribution half-life of 3.5 minutes and an elimination half-life of 27.5-28.2 hours. /Amphotericin B cholesteryl sulfate complex/ Following IV administration of conventional amphotericin B in patients whose renal function is normal prior to therapy, the initial plasma half-life is approximately 24 hours. After the first 24 hours, the rate at which amphotericin B is eliminated decreases and an elimination half-life of approximately 15 days has been reported. Elimination, half life: Neonates: Variable (range, 18 to 62.5 hours). Children: Variable (range, 5.5 to 40.3 hours). Adults: Approximately 24 hours. Terminal half life: Approximately 15 days. NOTE: There is large interindividual variation among neonates in the elimination of amphotericin B. Amphotericin B may persist in the circulation of neonates for up to 17 days after it has been discontinued. . The half life of elimination of amphotericin B from the lungs /of rats/ was 4.8 days according to serial sacrifices done after a single dose of 3.2 mg of aerosol doses of amphotericin B per kg. |
| Toxicity/Toxicokinetics |
Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Although no information exists on the milk excretion of amphotericin B, it is highly protein bound, has a large molecular weight, is virtually unabsorbed orally and has been use directly in the mouths of infants; therefore, most reviewers consider it acceptable to use in nursing mothers. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding Highly bound (>90%) to plasma proteins. Interactions Since nephrotoxic effects may be additive, the concurrent or sequential use of amphotericin B and other drugs with similar toxic potentials (eg, aminoglycosides, capreomycin, colistill, cisplatin, cyclosporine, methoxyflurane, pentamidine, polymyxin B, vancomycin) should be avoided, if possible. Corticosteroids reportedly may enhance the potassium depletion caused by amphotericin B and should not be used concomitantly unless necessary to control adverse reactions to amphotericin B. Antineoplastic agents (eg, mechlorethamine) may enhance the potential for renal toxicity, bronchospasm, and hypotension in patients receiving amphotericin B and such concomitant therapy should be used only with great caution. In a randomized, double-blind study that evaluated use of conventional IV amphotericin B and amphotericin B cholesteryl sulfate complex in febrile neutropenic patients with normal baseline serum creatinine concentrations, the incidence of renal toxicity (defined as a doubling or an increase of 1 mg/dL or more from baseline serum creatinine or a 50% or greater decrease from baseline in calculated creatinine clearance) was 31% in adults and pediatric patients who received amphotericin B cholesteryl sulfate complex concomitantly with cyclosporine or tacrolimus compared with 68% in those who received conventional amphotericin B concomitantly with these agents. In adults and pediatric patients who did not receive cyclosporine or tacrolimus therapy, the incidence of renal toxicity was 8% in those who received amphotericin B cholesteryl sulfate complex and 35% in those who received conventional amphotericin B. For more Interactions (Complete) data for AMPHOTERICIN B (15 total), please visit the HSDB record page. Non-Human Toxicity Values LD50 Mouse iv 4 mg/kg LD50 Mouse ip 88 mg/kg |
| References |
[1]. The antifungal drug amphotericin B promotes inflammatory cytokine release by a Toll-like receptor- and CD14-dependent mechanism. J Biol Chem. 2003 Sep 26;278(39):37561-8. Epub 2003 Jul 14. [2]. The effect of aggregation state of amphotericin-B on its interactions with cholesterol- or ergosterol-containing phosphatidylcholine monolayers. Chem Phys Lipids. 1997 Feb 28;85(2):145-55. [3]. Amphotericin B kills unicellular leishmanias by forming aqueous pores permeable to small cations and anions. J Membr Biol. 1996 Jul;152(1):65-75. [4]. Pharmacological studies of a new derivative of amphotericin B, MS-8209, in mouse and hamster scrapie. J Gen Virol. 1994 Sep;75 (Pt 9):2499-503. [5]. Amphotericin B encapsulated in micelles based on poly(ethylene oxide)-block-poly(L-amino acid) derivatives exerts reduced in vitro hemolysis but maintains potent in vivo antifungal activity. Biomacromolecules. 2003 May-Jun;4(3):750-7. |
| Additional Infomation |
Therapeutic Uses Ambecides; Antibiotics, Antifungal; Antibiotics, Macrolide; Antiprotozoal Agents MEDICATION: Antifungal; (VET): Antifungal MEDICATION (VET): ... Blastomycosis, histoplasmosis. Parenteral amphotericin B is used as a secondary agent in the treatment of paracoccidioidomycosis caused by Paracoccidioide brasillensis. /NOT included in US product labeling/ For more Therapeutic Uses (Complete) data for AMPHOTERICIN B (19 total), please visit the HSDB record page. Drug Warnings Rash (including maculopapular or vesiculobullous rash), purpura, pruritus, urticaria, sweating, exfoliative dermatitis, erythema multiforme, alopecia, dry skin, and skin discoloration or ulcer, have been reported in patients receiving amphotericin B. IV administration of conventional amphotericin B, amphotericin B cholesteryl sulfate complex, amphotericin B lipid complex, or amphotericin B liposomal may cause erythema, pain, or inflammation at the injection site. Phlebitis or thrombophlebitis has been reported with conventional IV amphotericin B. The manufacturer of conventional IV amphotericin B and some clinicians suggest that the addition of 500-1000 units of heparin to the amphotericin B infusion, the use of a pediatric scalp-vein needle, or alternate-day therapy may decrease the incidence of thrombophlebitis. Extravasation of the drug causes local irritation. Conventional IV amphotericin B is associated with a high incidence of adverse effects, and most patients who receive the drug experience potentially severe adverse effects at some time during the course of therapy. Acute infusion reactions (e.g., fever, chills, headache, nausea, vomiting) and nephrotoxicity are the most frequent adverse reactions to conventional IV amphotericin B. Although clinical experience with amphotericin B cholesteryl sulfate complex, amphotericin B lipid complex, and amphotericin B liposomal is limited to date, these drugs appear to be better tolerated than conventional IV amphotericin B. As with conventional IV amphotericin B, the most frequent adverse reactions to amphotericin B cholesteryl sulfate complex, amphotericin B lipid complex, or amphotericin B liposomal are acute infusion reactions; however, data accumulated to date indicate that lipid-based and liposomal formulations of amphotericin B may be associated with a lower overall incidence of adverse effects and a lower incidence of hematologic and renal toxicity than the conventional formulation of the drug. Acute infusion reactions consisting of fever, shaking chills, hypotension, anorexia, nausea, vomiting, headache, dyspnea, and tachypnea may occur 1-3 hours after initiation of IV infusions of conventional amphotericin B, amphotericin B cholesteryl sulfate, amphotericin B lipid complex, or amphotericin B liposomal. These reactions are most severe and occur most frequently with initial doses and usually lessen with subsequent doses. Fever (with or without shaking chills) may occur as soon as 15-20 minutes after IV infusions of conventional amphotericin B are started. The majority of patients receiving conventional IV amphotericin B (50-90%) exhibit some degree of intolerance to initial doses of the drug, even when therapy is initiated with low doses. Although these reactions become less frequent following subsequent doses or administration of the drug on alternate days, they recur if conventional IV amphotericin B therapy is interrupted and then reinstituted. For more Drug Warnings (Complete) data for AMPHOTERICIN B (18 total), please visit the HSDB record page. Pharmacodynamics Amphotericin B shows a high order of in vitro activity against many species of fungi. Histoplasma capsulatum, Coccidioides immitis, Candida species, Blastomyces dermatitidis, Rhodotorula, Cryptococcus neoformans, Sporothrix schenckii, Mucor mucedo, and Aspergillus fumigatus are all inhibited by concentrations of amphotericin B ranging from 0.03 to 1.0 mcg/mL in vitro. While Candida albicans is generally quite susceptible to amphotericin B, non-albicans species may be less susceptible. Pseudallescheria boydii and Fusarium sp. are often resistant to amphotericin B. The antibiotic is without effect on bacteria, rickettsiae, and viruses. |
Solubility Data
| Solubility (In Vitro) | DMSO :~50 mg/mL (~54.11 mM) |
| Solubility (In Vivo) |
Solubility in Formulation 1: 10 mg/mL (10.82 mM) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), suspension solution; with heating and sonication. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 100.0 mg/mL clear DMSO stock solution to 400 μL PEG300 and mix evenly; then add 50 μL Tween-80 to the above solution and mix evenly; then add 450 μL normal saline to adjust the volume to 1 mL. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 2: 10 mg/mL (10.82 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), suspension solution; with heating and sonication. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 100.0 mg/mL clear DMSO stock solution to 900 μL of 20% SBE-β-CD physiological saline solution and mix evenly. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. (Please use freshly prepared in vivo formulations for optimal results.) |